PROVIDER NETWORK OPTIMIZATION
Employed provider networks have become fundamental to hospital and health systems’ short- and long-term success. However, the placement of the employed network within a health system’s organizational structure has not evolved to reflect its importance. For example, while placement can vary widely across markets and systems, many networks are still buried as a hospital department under a layer or two of reporting seniors within the structure. Reviewing and potentially updating a network’s place in a health system can lead to improved performance, better morale, and a healthier bottom line. Download the PDF of the entire article.

“Multihospital health system organizational structures need to evolve to include the employed provider network as a peer of the hospitals and other organizational entities within the health system structure.”
Aligning Importance with Placement
In the recent past, it was common for an employed network to report into a senior executive (other than the CEO) who was already juggling multiple areas of responsibility. Even as the network grew and matured, the status and reporting relationship didn’t evolve, creating the impression that the network was subservient to and totally reliant upon others in the hospital for service support. This misperception extended from the network to the entire system. It’s critical that health systems looking to “bring together” their employed network of practices—transforming from a coalition of independent practices employed by the health system into a true multispecialty group with a common culture and vision— align placement with importance.
Specifically, multihospital health system organizational structures need to evolve to include the employed provider network as a peer of the hospitals and other organizational entities within the health system structure. In many cases, this change would result in significant elevation of the employed network’s status. The recommended placement depends on the complexity of the health system and the presence or absence of provider-based billing designations.
Figure 1: Executive Leadership Dyad Chart
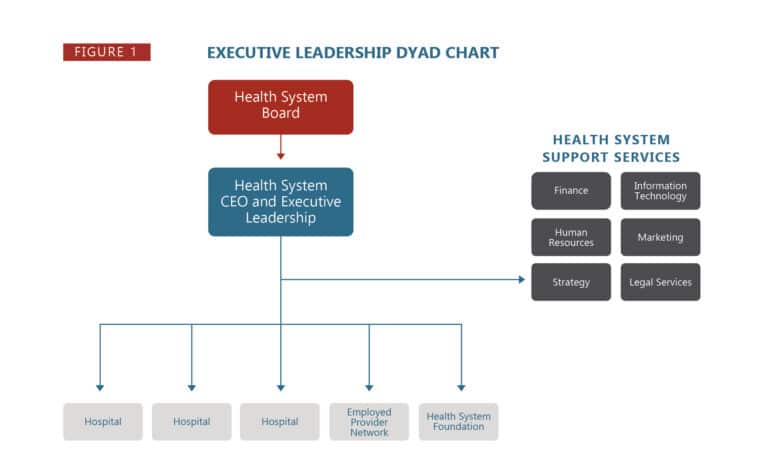
For optimal alignment, the Executive Leadership Dyad, shown above, should report to the health system CEO on the same level and in the same fashion as the designated hospital leaders. Corporate services that support all member entities, such as finance, human resources, revenue cycle, marketing, materials management, facilities management, and legal, should then reside at the health system level with tentacles of support permeating each of the supported entities. In this scenario, the employed network (considered Dedicated Support Services in the employed provider network organizational structure) is one of these supported entities. This organizational structure promotes optimal functionality and perceptions across the health system.
While an updated structure has long-term benefits, health systems initiating this type of structural change may initially face several potential obstacles for provider network optimization.
1) Acknowledging and changing the system’s culture and the mindsets of the health system members.
This process often requires leaders to completely reset frames of reference, and simply updating an org chart on a page is not enough. Many health system CEOs who are tasked with “systematizing” health system operations and functions encounter resistance from hospitals and hospital leaders who may maintain historic perceptions and competitive cultures. Overcoming individual identities and cultures can be a significant lift. Utilizing a shared vision process for the health system can bring a common roadmap and strategies to achieve greater unity—just as it can for employed provider networks facing similar situations. (1, 2, 3)
2) Developing “system” corporate support services that are truly housed, led, and operated at the health system level and not at the largest hospital level.
Raising these services and leadership teams to the corporate level improves perceptions of the network across the system and provides an environment for the network to continue to thrive.
3) Addressing the presence of provider-based billing in employed network offices.
Provider-based billing necessitates compliance with “hospital outpatient department” designation requirements for the involved practices. These requirements include specific licensure requirements, clinical services and reporting structure integration, financial accounting methodologies, and others. It’s possible that a health system may need to become a licensed entity with consolidated Boards, Medical Staffs (and Bylaws), and reporting structures reflecting and truly functioning in that fashion in order to manage and maintain compliance. Legal counsel guidance regarding this complicating factor is imperative.
Single hospital health systems also benefit from elevating employed network placement. Ideally, the employed provider network reports directly to the CEO (or COO if all other hospital entities report to the CEO through the COO) with the Executive Leadership Dyad included in hospital “C-Suite” membership.

Considering the employed network in this manner establishes its identity as a singular entity within the system with direct responsibility to the CEO. Challenges related to perceptual issues of status and of “adequate” shared services support may still exist and cultural changes may take a generation to fully evolve, but they can be more effectively addressed with this structure. Provider-based billing requirement compliance is also more easily managed in this structural recommendation.
Reviewing and evaluating the status of the employed network within the health system organizational structure is a critical step for health systems to take to remain competitive and operate with maximum effectiveness. This is especially the case when contemplating the status and adequacy of Dedicated Support Services within the employed network’s structure and function.4 By promoting a network to the organizational structure it deserves, healthcare leaders will set their health systems on a forward- looking path to ongoing success.
Contact HSG Advisors’ expert in employed provider networks and provider network optimization, Dr. Terrence R. McWilliams, MD, FAAFP at (502) 614-4292 or tmcwilliams@hsgadvisors.com.
References
1) https://hsgadvisors.com/white-paper/shared-vision-roadmap/
2) https://hsgadvisors.com/physician-leadership/employed-provider-network-shared-vision-process-and-intent/
3) https://hsgadvisors.com/physician-leadership/nine-elements-of-an-employed-physician-group-shared-vision/
4) https://hsgadvisors.com/articles/employed-provider-network-organizational-structure/
HSGadvisors.com | info@HSGadvisors.com © 2023 HSG. ALL RIGHTS RESERVED.