The 2022 CMS Split/Shared Visit Rules and the Anticipated Impacts

|
Download a PDF Version of the Article |
When many executives read reviews of the 2022 Medicare Physician Fee Schedule (MPFS) Final Rule, most focused on the additional 3.75% decrease in the Medicare conversion factor and the impact that determination would have on revenues. This focus is understandable considering the noteworthy 2021 increases in wRVU credit for many E/M and CPT codes and the subsequent monumental increases in production-based physician and advanced practice provider (APP) compensation for many specialties because of it – without a commensurate increase in professional services revenue.
The Split/Shared Visit rule changes included in the 2022 MPFS Final Rule could generate a similarly devastating disruption of wRVU credit, physician and APP compensation, and organizational revenue for hospital-generated professional services in many specialties.
WHAT PROMPTED THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES?
CMS previously defined the parameters for Split/Shared Visits in the Medicare Claims Policy Manual (Sections 30.6.1(B), 30.6.12, and 30.6.13(H)). When the Manual provisions were withdrawn on May 9, 2021 in response to petition, CMS indicated that it would update and clarify requirements through rulemaking. The 2022 MPFS presented that opportunity and the parameter changes are now codified in CMS Regulation § 415.140.
WHAT ARE THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES?
1) DEFINITION OF THE SPLIT/SHARED VISIT
The 2022 MPFS Final Rule defines a split (or shared) visit as “an E/M visit in a facility setting that is performed in part by a Physician and an NPP who are in the same group.” [NPP = nonphysician practitioner]
“Facility setting” is equated to an “institutional setting” in the Final Rule. According to the referenced regulation (§ 410.26(b)(1)), institutions are limited to hospitals and skilled nursing facilities (SNFs). The 2022 MPFS Final Rule added SNFs as a permitted location for Split/Shared Visits – with the impression that there would be close coordination and collaboration of care within groups providing care under these circumstances.
The 2022 MPFS Final Rule also clarified that the Split/Shared Visit scenario does not apply to the office setting. “Incident to” billing requirements would apply to office locations of care.
2) BILLING PROVIDER
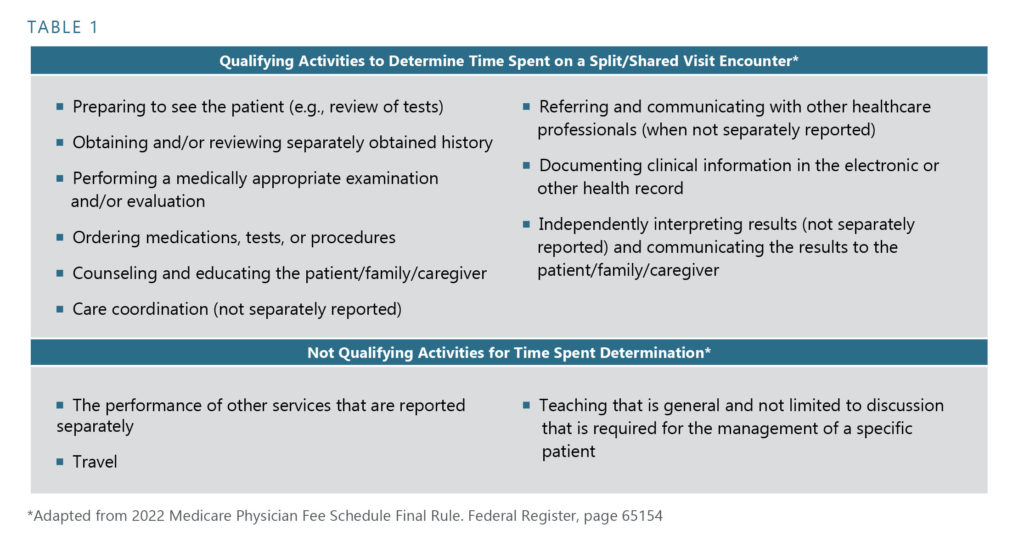
The 2022 MPFS Final Rule requires that the Split/Shared Visit encounter be billed under the provider who performed “the substantive portion” of the encounter. In the Final Rule, CMS intended to define the “substantive portion” of the encounter as being more than half of the total time dedicated to the patient encounter. The total time determination is defined similarly to the 2021 office-based coding requirements and is delineated in Table 1. Split/Shared Visit encounters can currently be billed under the involved physician as long as the physician’s “substantive” participation in the encounter was accurately documented in the medical record.
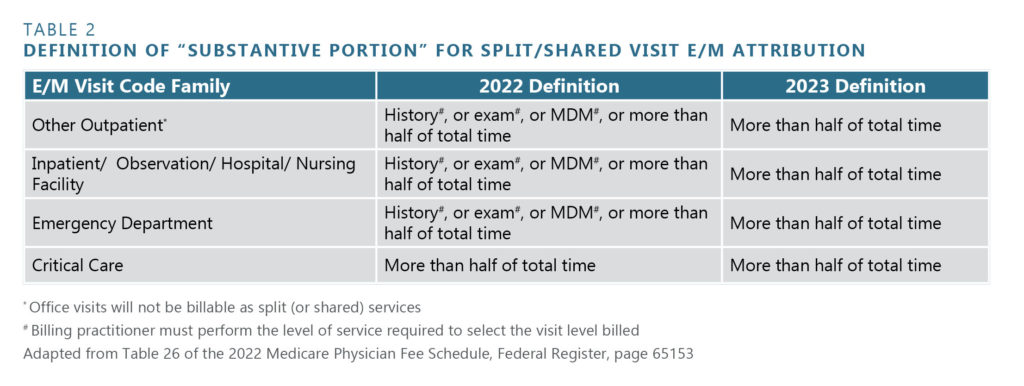
In response to public comment, CMS modified the effective date for implementing the intended “total time” definition as the sole determinant for “substantive portion” purposes and granted a transition year to allow a smoother conversion. “Total time” dedicated to the encounter will be the sole determinant effective January 1, 2023. For the CY2022 transition year, CMS will accept performance of history, exam, medical decision-making, or time spent as criteria – with the caveat that the billing provider must have performed the entirety of one of these first three elements to the degree that the visit billing level requires. Since critical care codes are based solely on time spent, dedicating more than half of the total time spent is the lone criterion effective January 1, 2022. The applicable determinants are summarized in Table 2.
In addition, the individual ascertained to be the “Billing Provider” is required to be the one that signs and dates the encounter document. The encounter document must clearly indicate the physician and APP involved in the patient’s care and their roles in that care – this includes the individual time and/or effort dedicated to the encounter in sufficient detail to justify the “Billing Provider” determination.
3) CLAIM SUBMISSION
In CY2022, Split/Shared Visit encounter claims must be annotated by a specific modifier – regardless of the provider type that the encounter is billed under. This permits identification and tracking of these encounters – something that was not able to be done in the past without performing manual record review. CMS felt that adding this identification factor would be important for ensuring program integrity (interpreted to imply that these claims can now actually be tracked and audited). After the Final Rule was published, MGMA reported that the designated modifier will be “FS.”
4) APPLICABLE ENCOUNTERS
The Split/Shared Visit criteria apply to new or established patients, initial and subsequent visits, critical care services, and prolonged services. Split/Shared Visit criteria could previously only be applied to “established” patient encounters.
WHAT IMPACTS WILL THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES HAVE?
In many hospital and SNF environments, APPs traditionally perform most of the time intensive aspects of Split/Shared Visit encounters. After all, this is one of the “values” of APP utilization in hospital settings – maximizing effective patient care delivery while efficiently minimizing dedicated physician time. Employed provider networks verify this is the case for many specialties, including hospital medicine. As a result, the above outlined changes create several important consequences.
1) WORKLOAD ATTRIBUTION/PRODUCTION-BASED PROVIDER COMPENSATION
Many employed provider networks directly attribute wRVUs generated by Split/Shared Visits to the “Billing Provider.” Under current circumstances, the “Billing Provider” is generally the physician as that designation allows “full” reimbursement for the professional services rendered to the patient by the care delivery team. Awarding all wRVU credit for Split/Shared Visits to the physician risks the perception that the physician is compensated for services that were not “personally performed” – a situation that is not fully aligned with Stark laws and regulations. One justification for the practice has been directly linking correlations with “incident to” scenarios. The distinction of Split/Shared Visits from office-based “incident to” circumstances in the 2022 MPFS places this justification in jeopardy.
Further, if the APP becomes the designated “Billing Provider” by performing the “substantive portion” of the encounter based on total time spent, the APP would, by the above default, be awarded all of the wRVU credit for these encounters. Awarding the physician these wRVUs would be very difficult to justify, as the physician did not perform a “substantive portion” of the encounter by definition. The immediate impact of this change is that the involved physicians’ wRVU credit would plummet – with serious consequences in production-based compensation models.
Consider the following options to address this new circumstance:
- If maintaining a production-based incentive remains an organizational imperative, create a teambased productivity incentive that pools earned wRVUs and distributes them equally among the involved physicians and APPs according to service or participation FTE. This option recognizes and promotes team member contributions to the overall group dynamics and successes while eliminating individual attribution issues and personally performed services concerns.
- If maintaining a production-based incentive remains an organizational imperative, create a mechanism to distribute wRVUs associated with Split/Shared Visits among the contributing individuals. This requires the ability to identify the individuals involved in each patient’s care and determining a fair distribution methodology. A 50/50 distribution methodology fully promotes a team-centered approach – although some organizations prefer to distribute according to the level of effort expended. This latter approach is more complex but more readily achievable with the new documentation requirements, i.e., how much of total time each participant dedicated to the encounter.
- If maintaining a production-based incentive is not an organizational imperative, consider eliminating the productivity component for shift-based providers, such as hospitalists, and incentivize nonproductivity elements like hospital clinical quality metric performance, committee participation, discharge summary completion, and others. Additional base income can be generated by covering more shifts and the individuals and the entire team can be incentivized to accomplish objectives that are actually within their sphere of influence.
2) MEDICARE REVENUE
As previously noted, most organizations designate the physician as the “Billing Provider” under current circumstances. This allows revenue generation at the lesser of 80% of the actual charge or at the fee schedule Amount for the services – essentially at 100% of anticipated revenue for the professional services rendered. hen an APP is the “Billing Provider,” revenue generation is at the lesser of 80% of the actual charge or at 85% of the fee schedule amount for the services – with the latter method predominating. The anticipated shift in “Billing Provider” designation noted above could result in the organization receiving 15% less revenue for the same volume and types of rendered professional services – and result in a significant loss of revenue for some specialties. This eventuality should be planned for, analyzed, and proactively addressed.
3) AUDITING ENCOUNTERS
Under current circumstances, payers do not require definitive identification of Split/Shared Visit encounters. This situation will change for submitted Medicare claims starting January 1, 2022. In the past, some organizations internally identified Split/Shared Visits in order to audit compliance and/or adjust workload attribution parameters. Some utilized a mechanism in which the physician was designated as the “Billing Provider” and the APP was designated as the “Rendering (or Service) Provider.” This system simultaneously identified the visit type and the involved physician and APP. These organizations often used this structure to not only audit encounters and ensure compliance with visit documentation requirements but also to individually attribute wRVU workload credit (often awarding a 50/50 split to promote true teambased function and performance). Others attached an internally derived modifier that was not reported externally to payers in order to identify these visits for internal audit purposes.
As alluded to above, CMS’ new requirement for adding a defined modifier to claims submitted for these visits allows them to be targeted for CMS audits. Developing or revising an internal audit process to ensure compliance with participation and documentation requirements would seem to be advisable.
CONCLUSION
Organizations need to be aware of the presence and potential impact of the new CMS Split/Shared Visit Requirements and proactively intervene to mitigate adverse consequences. With every challenge comes opportunity – and this challenge is no exception. Please feel free to contact HSG for analyses or assistance With any of these new issues – particularly the impact on physician and APP compensation models.
