|
Download a PDF Version to Share With Your Team |
“Our employed physician network is losing too much money” is a common refrain from
healthcare executives, many of which struggle to define an appropriate level of subsidy for their employed physician network. This lack of clarity is often coupled with no strategy for meaningful performance improvement of their employed physician network finances.
Then there are clients that are getting more specific. In a recent RFP, a health system defined their objective as halving the loss, cutting it from $24 million to $12 million. Framing the objective in that fashion is extremely helpful to us as consultants, causing HSG to sharpen its process to deliver the desired result.
Specific objectives help us determine the decisions that organizational leaders need to
make if they are to achieve that objective with our help. That framing helps us develop a realistic plan, as is pushes tough, and potentially costly, decisions to the front. That includes political decisions about services and specific physicians.
HSG has found it useful to evaluate collections and expenses per wRVU, define realistic objectives for each metric based on rigorous analysis, and tying that assessment to the subsidy objective.
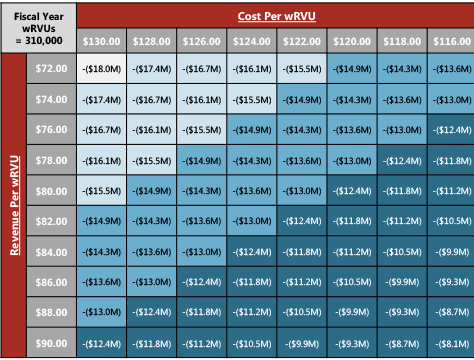
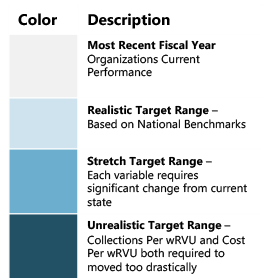
Networks seeking a 50% reduction in its overall employed physician network subsidy may find that it realistically can only cut 25% of its subsidy through operational improvement. The next step may be evaluation of divesture of providers or practices. This approach paints a clearer picture of what is realistic, and the underlying decisions required to drive improvement.
Factors Impacting Employed Network Financial Sustainability
For networks looking to improve financial performance, HSG utilizes a multifaceted approach centered around evaluating the network’s performance on a per wRVU basis. To achieve employed physician network “financial sustainability,” the network must focus on four areas:
- Collections per wRVU
- Expenses per wRVU
- Incremental Production of wRVUs with existing resources
- Divesture of Underperforming Practices or Providers

Improving Collections Per wRVU
Many networks struggling with financial performance focus on “cutting” their way to success – staff, management resources, etc. Maximizing revenue from the work currently being performed within the network is just as important as controlling costs. This is largely done through the following areas:
- Maximizing Commercial Payer Contract Rates
- Updating Fee Schedules
- Improving Payer Mix
- Improving Effectiveness of Revenue Cycle
- Coding and Documentation Improvements
Expenses Per wRVU
While maximizing collections is critically important, just as crucial is ensuring expenses per wRVU are being incurred at a sustainable rate. Improvements in expense per wRVU are generally found in the following areas:
- Aligning Provider Compensation with Production.
- Optimizing Provider Mix
- Utilizing Advanced Practitioners at Top of License
- Staffing Levels and Utilization
- Staffing Compensation
- Administrative Overhead Allocations
- Practice Overhead
- Practice Consolidation Opportunities
Incremental Production of wRVUs With Existing Providers
Even for networks struggling with maximizing collections per wRVU, generating more wRVUs with existing resources almost always generates a positive contribution margin. Typical gaps in maximizing wRVUs produced by a network’s current provider resources include:
- Retention of Patients / Network Integrity Improvement
- Maximization of Provider Schedules/ Templates
- Improving Patient Access
- Optimizing Practice Efficiency
- Top of License Provider Usage
- Maximization of Care Management Revenue Opportunities
- Improving Service and Procedure Mix
Divestiture of Underperforming Practices or Providers
Many networks struggling with financial performance are simply victims of employment decisions made over the past 10-15 years. The composition of employed networks that were built in the early-to-mid 2000s may not always be reflective of a health systems strategy today. In these cases, it makes sense to take a step back and evaluate the practices and providers that a network is subsidizing and ask, “why are we continuing to employ this practice?” Divestiture opportunities tend to present themselves in three ways:
- Mismatch between employment of the practice/specialty and the health system’s strategic needs
- Opportunity for the practice to move back to independence or join a loyal 3rd party, such as a local FQHC
- Realization that a practice will not be successful because of the physician’s weaknesses and/or demeanor
Pursuing Financial Sustainability
HSG partners with employed physician networks across the country to implement this type of analysis and move towards sustainable subsidies through performance improvement plans designed to improved employed physician network finances. HSG recently partnered with MGMA Connection Magazine to dive deeper into the issue of cutting employed physician network losses. For more information, contact Travis Ansel or David Miller.