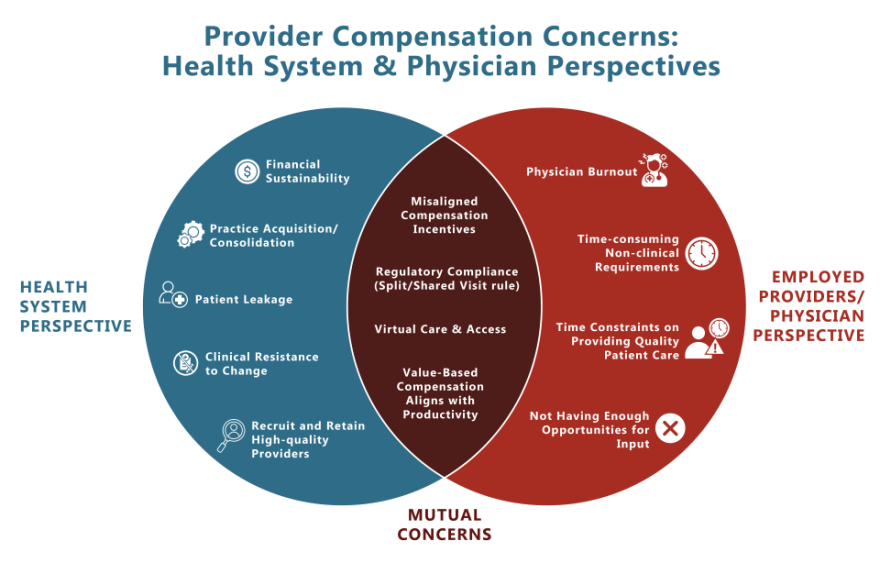
Physicians and Advanced Practice Providers (APPs) are the foundation of a health system’s ability to deliver quality patient care. Provider compensation models that 1) attract and retain high-quality providers while 2) meeting an organization’s operational, strategic, and financial targets are the goal of any health system.
Provider compensation is a multifaceted endeavor for all types of organizations; it involves balancing numerous objectives that may appear contradictory, such as strategic alignment, provider and market requirements, financial viability, and regulatory adherence. Despite its daunting nature, there are established best practices and successful approaches for devising comprehensive, sustainable, and efficient compensation strategies that cater to the needs of health systems and their employed provider networks.
Let’s delve into the five primary challenges health systems encounter in provider compensation and the practical solutions healthcare leaders can implement to construct effective compensation models:
- Challenge: Practice Acquisition/Consolidation
With the rapid acquisition and consolidation of independent practices into employed provider networks, health systems are charged with reconciling multiple disparate compensation models and expectations. Disjointed compensation across providers affects retention and is highly inefficient for network performance. Employed networks that aren’t well integrated can drag down revenue and performance.
Solution: Practice turnaround strategies can align different practices into unified, cohesive, and productive networks.
- Challenge: Value-Based Compensation vs Productivity
More and more employed provider networks are integrating value-based incentives into provider compensation models, but not necessarily at the expense of productivity. Striking the right balance between productivity models and non-productivity incentives is an ongoing and growing priority for healthcare executives.
Solution: As healthcare reimbursement models continue to evolve, compensation models, levels, and structures must evolve to be able to recruit and retain high-quality providers in an increasingly value-based environment.
- Challenge: Advanced Practice Provider Split / Share Visits
The 2022 Split/Shared Visit rule has had significant impacts on inpatient services’ wRVU credit, employed provider compensation, and health system revenue. Health systems are charged with navigating the effects of this rule and implementing practice changes accordingly.
Solution: Expert guidance on split/shared visits prepares healthcare leaders with information to address these changes effectively.
- Challenge: Financial Metrics and Incentives
An evergreen challenge for hospitals and health systems is aligning financial metrics and revenue goals with provider compensation incentives. Health systems are experiencing intensified competition for top talent and external financial pressures on their bottom lines.
Solution: Creative and flexible provider compensation plan designs can create compensation strategies that attract, reward, and retain physicians and APPs while meeting a health system’s financial targets.
- Challenge: Fair Market Value and Compliance
Without the right provider payment compliance, health systems face significant compliance risks. Optimizing provider compensation and minimizing risks encompasses compensation plan design, medical directorships, APP supervision, call pay, practice acquisitions, physician transactions, and more.
Solution: Fair market value and commercial reasonableness opinion reports are critical support and justification for each of the unique compensation models.
Provider compensation strategies are a key part of a larger whole for health systems. HSG looks across all areas of a health system to develop coordinated strategies—including compensation strategies. With HSG’s proprietary market and provider network data analytics and advisory services, healthcare leaders can better understand their markets and competitive influences, build effective strategic planning initiatives, monitor performance against defined objectives over time, and reassess and reprioritize on an ongoing basis.
There has been no shortage of external pressures on health systems and provider compensation over the past few years. Processes and approaches that worked effectively even five years ago have been rendered obsolete. Maintaining operational consistency and effective compensation plan design while adapting and adjusting to trends is more important than ever.
HSG partners with healthcare executives to design Physician and APP compensation plans that are flexible to ensure the network can remain financially sustainable, continually reflect the organization’s changes in culture and values, are regulatory compliant, and drive provider retention and engagement. With this approach, health systems benefit from more productive and engaged providers, stronger fiscal performance, and an even higher quality of patient care throughout changes in market forces and organizational goals and objectives.
