Physician Leadership Within Employed Provider Networks.pdf
Physician Leadership Within Employed Provider Networks.pdf |
Download a PDF of this article to share with your team |
INTRODUCTION
Physician leadership has long been an important entity in health systems, but it is receiving heightened attention on the journey to value-based care. Physician leadership at all levels and in all settings is indispensable to realizing success with achieving high quality, safe patient care in the most cost-effective manner in an employed physician network. Not to mention the importance of high patient engagement in and satisfaction with the care provided. Not only is most of the direct patient care delivered in America delivered or influenced by physicians, but peer-to-peer physician interactions have proven to be the most effective mechanism to influence physician behavior.
INCORPORATING PHYSICIAN LEADERSHIP INTO THE ORGANIZATIONAL STRUCTURE
In our experience1, incorporating physician leadership into the organizational structure and within the fiber of employed physician network function propels the employed network forward on its Growth Curve path – improving performance, increasing strategic value, and achieving high performance. The impact on the physician network exceeds that afforded through the delineated structural elements and includes the following additional benefits:
 | Engagement Directly involving physicians in the problem-solving and decision-making process engages them in the network’s work product and instills a sense of ownership in the outcomes – something that employment alone fails to accomplish. |
 | Alignment Direct involvement in establishing and collaborating with program, and related project, development enhances the likelihood of alignment (and engagement). Creating this level of alignment then permits formal incorporation of associated incentives within the compensation plan, which further cements the interrelationship. |
 | Retention and Recruitment As physicians become involved, aligned, and engaged with network strategies and tactics, the work environment favorably evolves to enhance physician job satisfaction – and network reputation as a preferred place in which to practice. Consequently, retention rates and recruitment successes improve. |
 | Burnout Mitigation Promoting direct physician input into practice and group operations is one of three categories of organizational initiatives that can reduce the risk of physician burnout within the network. |
Because of its global impact on network function, HSG identifies Physician Leadership as one of eight key elements that produce employed physician network success,3 or a high-performing physician network. It is intimately intertwined with initiatives accomplishing favorable outcomes related to each of the other elements. The importance of aligned physician leadership cannot be overemphasized as physician passivity, or outright antagonism, makes systemic dysfunction inevitable. Thus, the return on investment in physician leadership can be profound.
To be successful, organizations must cultivate key physician leaders who understand clinical, market, and economic issues; who are committed to improving quality; who are willing to model and drive desired culture; and who are willing and able to hold peers accountable. These individuals must embrace the role of rallying peers and colleagues to accept the challenges associated with the evolving healthcare environment and actively leading positive change.
Physician leaders must represent a philosophy that balances individual autonomy with system expectations; advocates for both the patient and the system; adeptly promotes team participation; and leads by example. They help to establish direction, buoy the vision, and align, motivate, and inspire others to follow. These tenets apply to all levels of physician leadership – from front-line leadership at the point of care to middle management and senior management.
Successful progression along the physician leadership continuum must be cultivated through active coaching and mentoring, formal didactic programs, and self-learning adjuncts. All contribute to individual skill enhancement to be able to effectively plan, organize, empower, and problem-solve. These deliberate interventions augment experiential learning – the value of which should not be underestimated. Progress depends on developing and expanding both leadership and management skills.
To attain the greatest benefit, employed networks must embed physician leaders in the formal management infrastructure and not rely solely on informal influence to effect change. Two primary mechanisms through which this can be accomplished include creating formally designated physician leadership positions in the organizational chart and establishing a physician leadership council. Each of these approaches provides direct physician input into the organization’s strategic planning and operational problem-solving and decision making processes.
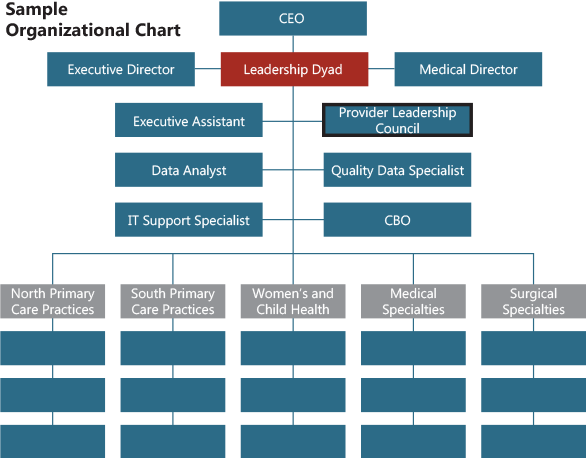
Formally designating physician leadership positions in the organizational chart most often refers to a Chief Medical Officer or Medical Director position for the employed physician network as a senior leadership position; regional or divisional medical directors as middle management positions in large networks; and lead physicians of large practices as early middle management positions with significant front-line leadership roles.
Rather than creating isolated physician leader positions, networks should consider pairing a physician leader with an administrative leader in a dyad management team structure.4,5,6 Dyads can be a highly productive and efficient leadership tandem in which both individuals have primary and shared responsibilities that exploit personal and professional strengths to result in synergistic function and shared accountability for performance. Note that dyad partners complement each other, function collaboratively (not in isolation), and act in concert as a partnership team. Although each member has delineated individual and shared responsibilities, successful dyads continually discuss issues and challenges so that the strengths of each contribute to the most favorable outcomes. The dyad structure is applicable at all levels of network leadership.
Like all aspects of leadership, effective dyads are cultivated. Creating a true dyad management team requires more than just naming individuals to the positions and assuming they will function as desired. The concept represents a paradigm shift from traditional interactions to additional training or coaching being required to achieve the desired level of interactive functionality.

When properly implemented and executed, physician/administrator dyad management teams can have a profoundly positive impact on organizational success.
Establishing a Physician Leadership (or Advisory) Council is another crucial mechanism to incorporate physicians (and APPs, which can alter the designation to Provider Leadership Council) into network planning, problem-solving, and decision-making processes. This mechanism can be organized and implemented in a relatively short span of time and in a cost-effective manner. Physician Leadership Councils should be established through a Charter that defines its composition, leadership, functions, term limits, and reporting requirements. Council functions often include the following:
Solicit strategic and tactical input from direct care providers. Early, ongoing physician involvement in the strategic planning process predicts more positive results.
Review practice performance. Established operational (financial, productivity, and efficiency), clinical quality, patient safety, and patient satisfaction metrics should be reviewed through a dashboard format on a regularly-scheduled basis. This provides the opportunity to replicate positive practices and identify potential areas for improvement.
Present potential new initiatives.The Council is an excellent place to vet proposed initiatives arising from management or from the practices.
Promote physician “ownership” of practice function and initiatives. Abdicating, or abrogating, this important responsibility will result in subpar performance.
Establish the desired culture. The Council creates the foundation for a common culture within the network and Council members serve as role models for peers and colleagues.
Educate and groom future leaders. Council membership introduces prospective leaders to the network/hospital/health system’s perspective and promotes a collective rather than individual focus that can differentiate potential leadership candidates and allow early development of leadership characteristics.
The ideal Physician Leadership Council membership should be relatively inclusive to achieve the broadest input during Council deliberations and effect the greatest acceptance for Council decisions balanced against being small enough to effectively make decisions. The membership should be representative of the network’s specialty mix, geographic locations, ages and experience levels, gender, and APP mix.
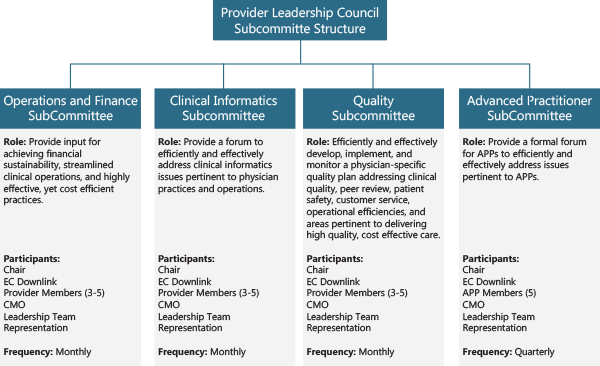
Even the most effective Councils cannot deal with all details associated with their broad responsibilities and often create a committee structure to do so. In this manner, the multidisciplinary Committees perform the detailed work related to their defined area of responsibility on behalf of the Leadership Council and report its efforts directly. Another benefit of the Committee structure is affording additional opportunities to involve more group members in network operations, promoting engagement and “ownership” within the group.
Committees are established in a similar manner to the parent Council – with a defined charter or charge. Common functional areas guiding Committee formation include Quality, Clinical Informatics, Operations, and Finance. In addition, many networks develop constituency committees to represent the professional concerns and development of members – most commonly applied to APPs.
Committee function must remain intimately linked to Council function. One mechanism to accomplish this objective is designating a Council member to be a downlink (liaison) from the Leadership Council to a Committee. This position ensures direct, first person knowledge of both Physician Leadership Council and Committee workings, deliberations, and processes. A second mechanism to accomplish this objective is to have the same organizational leader(s) (i.e., the network dyad management team) designated as a member(s) of each Committee. This element also ensures a common direction is maintained across all functional areas.
Finally, committee function should also be linked with the corresponding hospital/health system program(s) to avoid siloed functions. This linkage is usually accomplished through a combination of committee membership designation and process development.
CONCLUSION
Investing in developing and involving physician leadership at all levels and aspects of the organization will reap broad benefits, including more closely aligning physicians with the organization.
Physician leadership should be formally incorporated within the organization’s management infrastructure by formally designating physician leadership positions and establishing a physician leadership council to provide direct input into the organization’s strategic planning and operational problem-solving and decision-making processes. Doing so will lead to more efficient and effective organizational function, enhanced positioning for value-based care delivery, and accelerated progress toward becoming a high performing network.
GETTING STARTED
HSG can assist with incorporating physician leadership within employed provider networks – particularly with creating, optimizing, or re-organizing Provider Leadership Councils. We possess extensive experience in this area and maintain a wealth of customizable documents and processes to effectively facilitate and catalyze the process to achieve tangible results in a compressed time frame.
CITED REFERENCES
1. D.W. Miller, et al, Employed Physician Networks: A Guide to Building Strategic Advantage, Value, and Financial Sustainability. Health Administration Press, 2019.
2. Mitigating Physician Burnout: Developing a Proactive Organizational Approach. HSG
https://hsgadvisors.com/thought-leadership/white-paper/physician-burnout/3. 8 Keys to Building a High-Performing Employed Physician Network. HSG
https://hsgadvisors.com/thought-leadership/articles/8-keys-building-high-performing-employed-physician-network/4. D. Zismer, J. Brueggemann, Examining the “Dyad” as a Management Model in Integrated Health Systems. PEJ, January/February 2010.
5. K. Baldwin, et al, Health Care Leadership and the Dyad Model. PEJ, July/August 2011.
6. G. Barnhart, M. O’Brien, Administrator-Physician Dyads: High Potential, High Risk. Executive Brief.