Download the PDF of this case study.
INTERIM LEADERSHIP AND REVENUE CYCLE OVERVIEW
A Regional Medical Provider faced provider-based billing challenges and needed support with rural health certifications for some of its practices.
System leaders reached out to HSG Advisors to help launch two rural health care clinics and nine hospital-based billing departments (HOPD)
because they were losing revenue due to lack of patient/customer access and inefficiencies in its coding and billing practices.
HSG performed a holistic assessment of the health system’s operations, and identified critical success factors, challenges, and opportunities. After HSG’s initial 90-day project management engagement, the system leaders asked HSG Advisors to provide additional services, including revenue cycle management and an interim leadership role. Through a collaborative partnership with HSG, the health system enjoyed significant improvements to its bottom line.
CHALLENGES
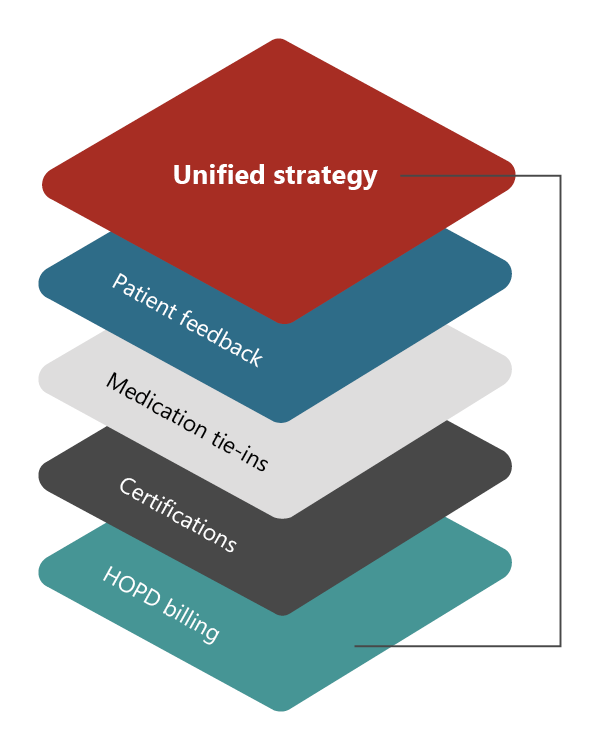
The Health System team needed assistance bringing together multiple operational touchpoints (HOPD, certifications, billing) into a cohesive strategy. However, after the initial analysis, it was determined that additional opportunities could be uncovered with ancillary services from HSG.
SOLUTIONS
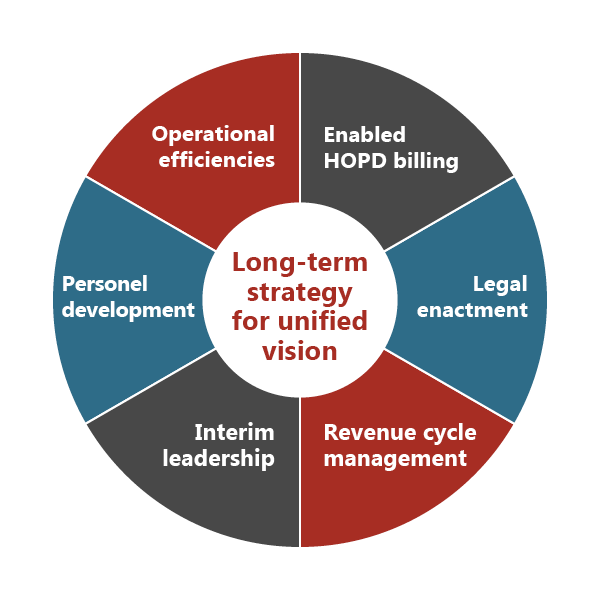
HSG developed a long-term strategy by conducting a custom analysis of the Health System, creating a unified vision, and identifying an integrated series of tactics to fulfill the strategy based on the Health System’s comprehensive and unique needs.
APPROACH
Increased Operational Efficiencies
■ Independent coders were brought in to perform chart audits
■ Coders read documentation and performed analyses to determine where revenue was being left on the table, including the “what” and the “why”
■ Operational components and facilitated computer conversions were set up to enable HOPD billing
■ Strategies set up to ensure doctors and key staff were getting feedback
■ Set up $340B in medication tie-ins (related to the Ryan White Act)
■ Partnered with the Health System’s leaders to initiate programs based on measurable metrics, such as wait times
Improved Personnel Development
■ C-suite level interim leadership with an onsite consultant
■ Participated in system-specific training and provided education to staff on updated policies and practices
■ Utilized shared culture and physician engagement practice strategies to ensure the doctors and key staff positions were on board, getting feedback, participating in training
■ Conducted training and evaluations
Established Measurable Policies
Key to the Health System’s success was implementing the No Surprise Billing Act.
■ Policies and software systems were set up to support the Health System’s leaders with this critically important process to ensure compliance and allow staff to focus on patient care rather than billing red tape.
■ The HSG team helped managers initiate policies and procedures based on measurable metrics within their programs, such as wait times.
■ When new guidelines were published (due to an IRS mandate), HSG led the roll outs and updates, including:
■ The IRS mandate now requiring health systems provide uninsured or out-of-network
patients with a cost estimate within 4% of the actual billing charge.
■ Setting the Health System up to run audits for these billings and has a point person established for policy reevaluations.
RESULTS
The Health System continues to see bottom line improvements on the financial side. The new billing implementation began to reverse previous losses and there is a new revenue source from the additional HOPD ROI.
SERVICES PROVIDED
■ Interim leadership
■ Hospital-based billing department consulting
■ Rural health care strategy
■ No Surprise Billing Act guidance
■ Revenue cycle management
Download the PDF of this case study.
