
|
Download a PDF Copy to Share With Your Team |
On March 17th, CMS announced that it would expand reimbursement for telehealth interactions involving Medicare beneficiaries during the COVID-19 pandemic. The expansion applies to care normally rendered in offices, hospitals, and skilled nursing facilities and helps to offset revenue losses incurred with the elimination of non-urgent encounters effective with the March 18th notice.
CMS previously only reimbursed for virtual encounters in designated rural environments and the patients had to be physically present in a healthcare facility during the interaction. With the COVID-19 pandemic impact, CMS re-emphasized the programs initiated during the 2019 and 2020 Medicare Physician Fee Schedule Final Rules and expanded its prior telehealth reimbursement rules. The CMS Fact Sheet can be accessed at www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet.
The following outlines various telehealth reimbursement requirements:
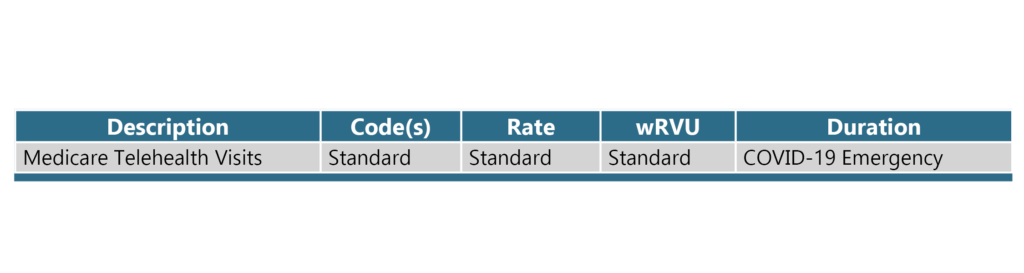
MEDICARE TELEHEALTH VISITS
Telecommunication technology may be used for office, hospital, and other services provided for Medicare patients that would generally occur in person within the following guidelines:
- The provider must use an interactive audio and video telecommunications system that permits real-time communication between the provider and the patient at home.
- Eligible provider types can include physicians, nurse practitioners, physician assistants, nurse midwives, certified nurse anesthetists, clinical psychologists, clinical social workers, registered dietitians, and nutrition professionals.
- The audio and video telecommunications systems that can be used have been expanded to include everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency.
- The virtual visits will be considered to be equivalent to and reimbursed as face-to-face encounters. The full spectrum of applicable codes can be found at ww.cms.gov/Medicare/Medicare-General-Information/ Telehealth/Telehealth-Codes.
- Medicare co-pays and deductibles apply to each of the virtual encounters – although they are allowing providers to have flexibility to reduce or waive these fees for the virtual encounters if desired.
- These opportunities are intended to apply to established patients, but HHS will not audit the process – i.e., can be used for new patients as well as established patients during this crisis.
- The applicability is retroactive to encounters occurring since March 6th.
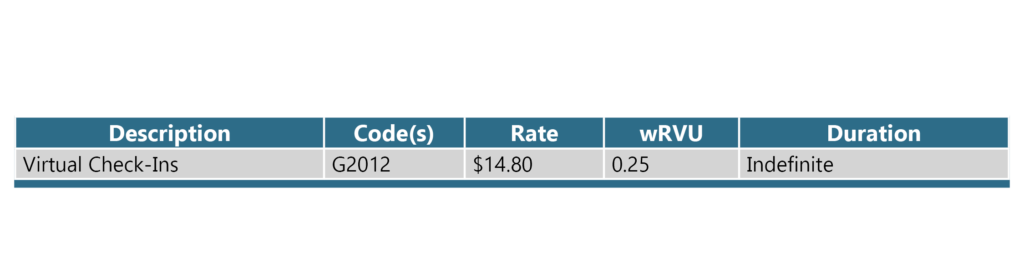
VIRTUAL CHECK-INS
Established in the 2019 Medicare Physician Fee Schedule Final Rule and apply even after the COVID-19 national emergency abates. Must meet the following requirements:
- Applies only to established patients.
- Must be patient initiated contact – usually via telephone – although practices are permitted to educate eligible beneficiaries about its availability and requirements … even during the telephone consultation process.
- The patient must verbally consent, which must be documented in the medical record.
- Medicare co-pays and deductibles apply.
- Providers can respond via any modality such as telephone, secure test messaging, secure email, or patient portal.
- The “Virtual Check-In” parameters include:
- Cannot originate from an E&M service in previous 7 days
- Cannot lead to an E&M service or procedure within the next 24 hours or the soonest available appointment from the interaction
- Assumes 5-10 minutes of medical discussion by a credentialed provider
- Coded as G2012.
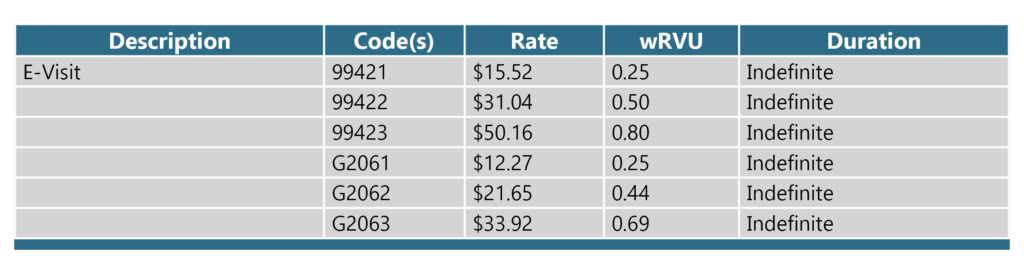
E-VISITS
Established in the 2020 Medicare Physician Fee Schedule Final Rule and apply even after the COVID 19 national emergency abates. Many of the same requirements for “Virtual Check-Ins” apply as this is essentially a “Virtual Check-in” through an online patient portal and permits tiers payment based on cumulative time expended.
- Applies only to established patients.
- Must be patient initiated contact through an online patient portal. Practices are permitted to educate eligible beneficiaries about its availability and requirements.
- The patient must verbally consent, which must be documented in the medical record.
- Medicare co-pays and deductibles apply.
- Provider responds via the online patient portal.
- The “E-Visit” parameters include:
- Cannot originate from an E&M service in previous 7 days
- Cannot lead to an E&M service or procedure within the next 24 hours or the soonest available appointment from the interaction
- “E-Visit” claims submissions are based on the rendering provider type and the cumulative time invested during a 7-day interval starting from the initial patient contact.
- Practitioners who may independently bill Medicare for evaluation and management visits (e.g., physicians, APRNs, PAs) can bill the following codes:
- 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes
- 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes
- 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes
- Clinicians who may not independently bill for evaluation and management visits (e.g., physical therapists, occupational therapists, speech language pathologists, clinical psychologists) can bill the following codes:
- G2061: Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5–10 minutes
- G2062: Qualified non-physician healthcare professional online assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 11–20 minutes
- G2063: Qualified non-physician qualified healthcare professional assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes
- Practitioners who may independently bill Medicare for evaluation and management visits (e.g., physicians, APRNs, PAs) can bill the following codes:
Other pertinent telehealth situations established in the 2019 Medicare Physician Fee Schedule Final Rule and apply even after the COVID-19 national emergency abates include the following:
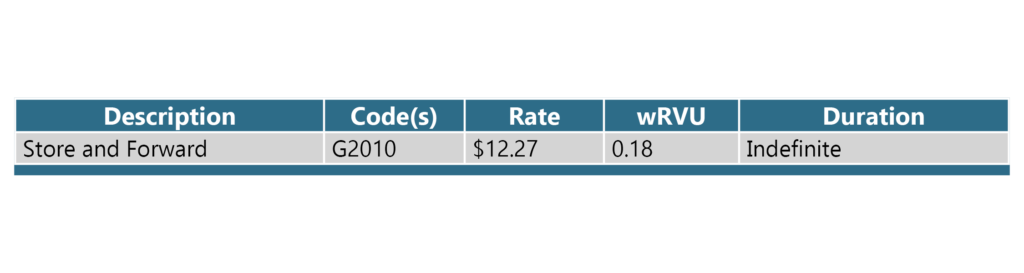
“STORE AND FORWARD” COMMUNICATION
- Remote evaluation of recorded video and/or images submitted by an established patient through asynchronous transmission of health care information.
- Permits provider payment when a patient submits a photo or video information to evaluate the patient’s condition or to assess whether a visit is needed.
- All requirements and parameters of a “Virtual Check-In” apply.
- Coded as G2010.
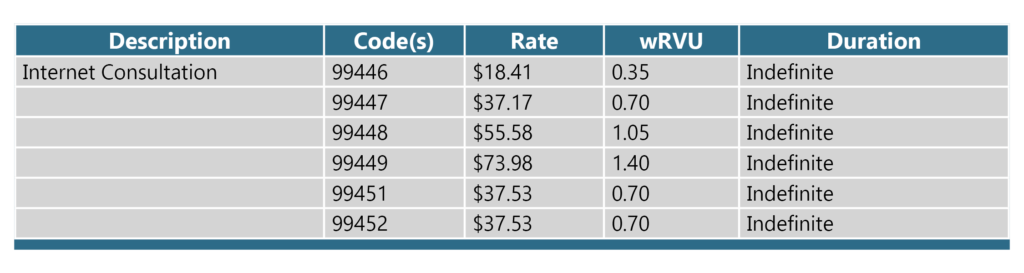
INTERPROFESSIONAL INTERNET COMMUNICATION
- Establishes payment for telephone, internet, or EHR interprofessional consultations when the treating provider requests the opinion and/or treatment advice of a consulting provider with specialty expertise to assist with the diagnosis or management of a patient’s problem without the need for face-to-face patient contact with the consulting provider.
- The following codes apply to this situation
- 99446 – 5-10 minutes of discussion or review
- 99447 – 11-20 minutes of discussion or review
- 99448 – 21-30 minutes of discussion or review
- 99449 – 31 minutes of discussion or review
- 99451 – Consultant provides a written report to the requesting provider and involved five or more minutes of consultative time
- The following codes apply to this situation
- Establishes reciprocal payment for treating provider the when the consultant requests similar information from the treating provider.
- The following code applies to this situation:
- 99452 – Provided by a treating/requesting provider; 30 minutes
- The following code applies to this situation:
- The patient must verbally consent to this type of interaction and the consent must be documented in the medical record.
- Medicare co-pays and deductibles apply.
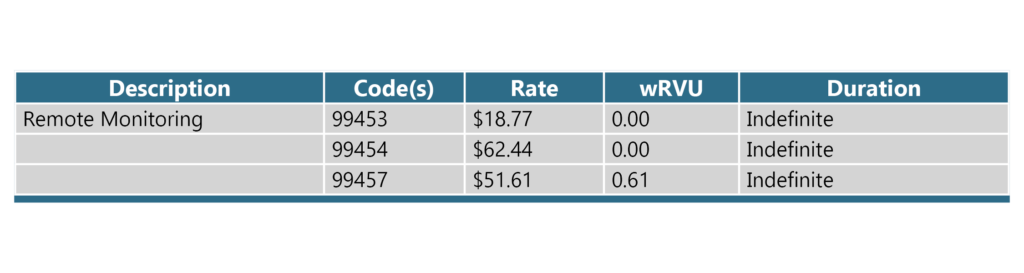
CHRONIC CARE REMOTE PHYSIOLOGIC MONITORING
CMS created three (3) new CPT codes to allow payment for set-up, technical supply, and treatment management services when furnishing remote patient monitoring (RPM) services.
- 99453 – For the set-up and patient education on the use of RPM device(s).
- Reported once for each episode of care beginning when the remote monitoring service is initiated and ending with attainment of targeted treatment goals.
- 99454 – For the monthly supply of device(s) for daily recording(s) or programmed alert(s).
- 99457 – For clinical staff/physician/other qualified health care provider remote physiological monitoring treatment management services of a patient under a specific treatment plan.
Pertinent telehealth situations established in the 2020 Medicare Physician Fee Schedule Final Rule and apply even after the COVID-19 national emergency abates include the following:
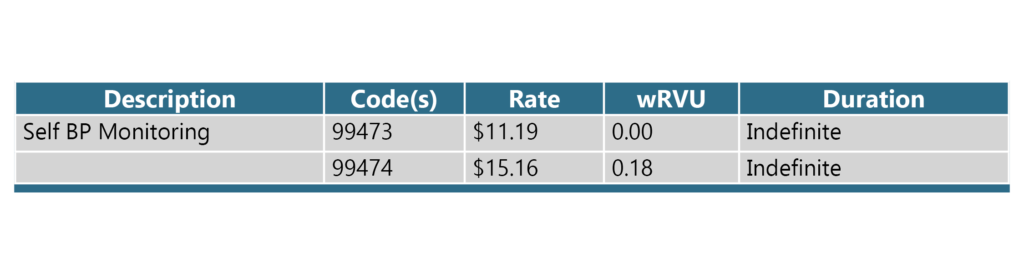
SELF-MEASURED BP TREATMENT PLAN SUPPORT
CMS created three (3) new CPT codes to allow payment for set-up, technical supply, and treatment management services when furnishing remote patient monitoring (RPM) services.
- 99473 – Self-measured BP using a device validated for clinical accuracy. Includes patient education/ training and device calibration.
- 99474 – Separate self-measurements of two readings one minute apart, twice daily over a 30-day period (minimum of 12 readings), collection of data reported by patient or caregiver to the provider, with report of average systolic and diastolic pressures and subsequent communication of treatment plan to the patient.
- Caveats:
- Cannot be in same calendar month as ambulatory BP monitoring
- Cannot be reported in conjunction with remote monitoring codes
Now is probably the best opportunity to initiate virtual care – and get reimbursed for those efforts. Please let us know how we can help in your efforts by contacting Dr. Terry McWilliams.
