One of health reform’s goals is to change the way health care is delivered in America. Rather than treating patients in silos, health reform initiatives encourage providers to work together. Cancer care is an excellent example of the need for a team approach to care. Because it can involve many silos – medical oncology, radiation oncology, surgery, radiology/imaging, pathology, clinical trials, home health, hospice – the American Society of Clinical Oncology (ASCO) and the American College of Surgeons Commission on Cancer (ACS/CoC) have long promoted a multidisciplinary team approach.
Understanding Co-Management Agreements
How do you transition coordinated cancer care from a buzzword to a reality? A good place to start is with a “co-management agreement” – a formal contractual relationship whereby a hospital contracts with a group of physicians to help manage a service line. The intent is to align hospital and physician goals to improve quality and reduce costs.
From a compensation perspective, co-management agreements consist of two components:
- Base fee built on hourly rates and physician time devoted directly to managing the service line, and
- Incentive fee tied to quality, customer service, programmatic milestones and efficiency goals.
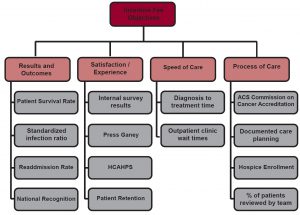
Base fees are fairly standard, typically $125-$200 per hour. It’s the incentive fee that can be tailored to promote coordinated care and other program goals. The flowchart below offers general objectives to keep in mind when developing incentive fees for oncology service line co-management agreements:
Eight Steps to Developing Incentive Fees That Get Results
- Determine your vision for your program.
- Decide what you want to accomplish in the short term and long term.
- Involve physicians from the beginning of the process all the way through selection of the metrics and targets.
- Select metrics that incentivize physicians to help you meet your immediate goals and simultaneously make it possible to achieve the long-term vision.
- Keep it simple. Select less than 10 (the ideal is five to seven) metrics for your incentive component.
- If possible, at least half of the metrics should be recognized by the National Quality Forum (NQF) and authored/sponsored by organizations such as ASCO and ACS/CoC and should be based on achieving or exceeding national benchmarks.
- All targets should be “stretch” goals, reasonably attainable but not “layups” for the doctors. If reaching national benchmarks isn’t reasonable or enough of a stretch, develop incentives that reward significant improvement over historical/ baseline performance.
- Keep your eyes on the prize: the impact that reaching the cancer program’s shared vision will have on the physicians’ professional reputations, the program’s success, and the lives of the people you serve.
