While the definition of Population Health Management (PHM) may not always be perfectly clear, what IS clear is that pursuing a PHM strategy requires a total redesign of traditional healthcare delivery and payment systems.
What is Population Health Management?
PHM is one of the core tenets underlying the current healthcare reform movement. The term, or variations of it, finds its way into a number of care models and reform initiatives, namely:
- The Triple Aim initiative
- The Value-Based Care Organization (ACO) concept
- The Patient Centered Medical Home (PCMH) model
Before evaluating the requirements for competing in this new environment, it’s important to draw a distinction between the many terms used in reference to PHM. The Institute for Healthcare Improvement (IHI) and other groups offer some insight.
IHI considers population medicine to be the “design, delivery, coordination, and payment of high quality health care services to manage the Triple Aim for a population using the best resources” available within the healthcare system. Population medicine requires a comprehensive approach to care embodied in methodologies such as ACOs, PCMHs and new chronic condition care models.
Population management is the structure supporting population health initiatives: reimbursement models and shifting provider alignment from care provided and paid for at an individual level to managing and paying for the total cost of care for a defined population.
Population Health can be defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group. These groups are often geographic populations such as nations or communities, but can also be other groups such as employees, ethnic groups, disabled persons, or any other defined group.” [1]
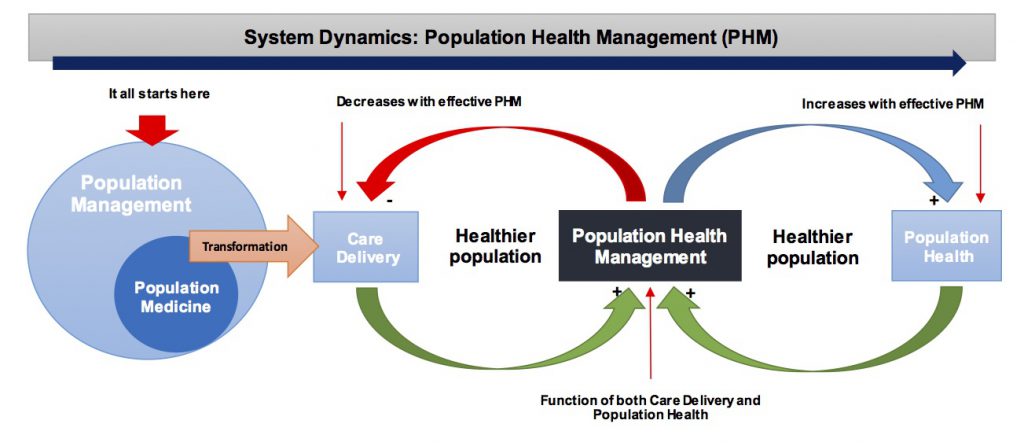
Population health management is the union of the structural system aspects of population management and population medicine with the clinical goals targeted by population health initiatives. As shown in the System Dynamics diagram (left right above below), it creates balance among the often competing interests and tactics of population medicine, population management and population health.
PHM’s Three Core Requirements
- Altered Primary Care Models
A strong primary care base is the foundation of PHM. Because primary care forms the nidus of patient interactions and care coordination, practice capabilities must be redefined to support population health management strategies. A good starting point is embracing the PCMH model.
- Extensive Data and IT Support
PHM requires a single data repository that integrates clinical, financial and utilization data from multiple sources across the medical community. This comprehensive view of a patient’s health status is critical to managing care across the full continuum and ensuring patients receive the right care in the right venue at the right time. Advanced data analytics are required to risk stratify the patient population, devise comprehensive care management programs, manage costs and utilization, create disease registries and track progress on quality indicators.
- Patient and Community Engagement
To be truly effective, population health management initiatives must “touch” two groups: patients who actively seek care and patients who don’t. While care management resources are key, innovative programs will be required to effectively reach both groups. Many experts feel that engaging patients in their own care processes will be the lynchpin to successfully transforming care.
Developing Your Strategy
Population medicine and population management are key to redesigning the current volume driven care delivery system to a system driven by quality, outcomes and shared accountability. This is where it all starts for provider organizations that have embraced population health management, and are seeking ways to compete in this new environment.
Clinically Integrated Networks (CINs) are well positioned to pursue population health management initiatives. They align the clinical and financial interests of hospitals and employed physicians with the broader independent physician community under a common infrastructure. As a single entity, the CIN is capable of managing an array of value-based payment arrangements and as well as benefits from joint contracting opportunities that result from delivering greater value through a demonstrated ability to improve care and control costs.
[1] David Kindig’s definition of Population Health
