Before you answer this question, consider the following:
- A high-performing physician network is a strategic asset that must lead the way for clinical integration. If your group fails to meet its potential, your hospital risks becoming a second-tier player.
- CMS payment schemes: bundled payments, PCMH’s MIPS, and ACOs will require drastic changes in the way patient care is delivered. The skill sets required to manage the group and the practices have changed. Attracting and retaining capable people will be much more difficult as market demand outstrips the supply.
- Network management experts can help you avoid costly errors.
- Improving care and managing costs demands a strong partnership with your physicians. Your physician group should be the catalyst and lead these initiatives. Often though, the physicians don’t understand their role in this process.
- It is likely that you have made a sizable investment in building and operating your physician group. With practice losses growing and threatening to wipe out hospital margins, hospital boards are demanding answers. You can’t afford mistakes at this point.
Building an employed physician network is an “All-In Bet”. There is no turning back at this juncture. You’ve got to get this right!
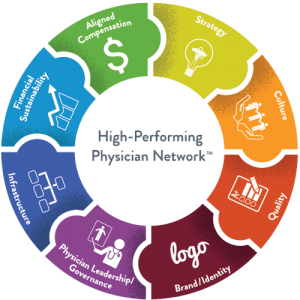
As we see it, you have two options: Either build the management team and infrastructure internally, or outsource to a firm specializing in managing and operating physician groups and their transition to clinical integration. Using a firm that specializes in operating physician groups is a wise choice, particularly as the group evolves and grows in complexity.
The following summarizes the Pros and Cons of Out-Sourcing:
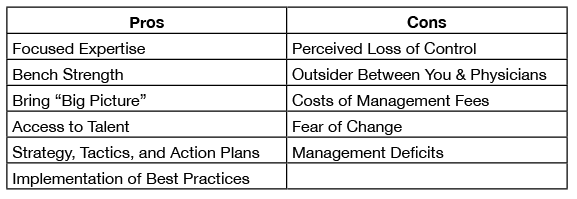
The Cons are legitimate concerns. The most pressing issues are the perceived loss of control and having an “outsider” between the executive team and the physicians. However, these don’t have to be negatives. Rather, positioning the management firm and their team as dedicated resources to the group reinforces the C suite’s commitment to the physician group. This defuses the perception by the physicians that they are treated as “second class citizens”.
While change can be daunting and may result in anxiety at the physician level, having a team on-site managing day-to-day operations using proven best practices will usually quell these fears. And taking decisive action to go outside for professional management shows the board that you are committed to improving group operating results and integrating the group into the hospital and health system. You are not admitting failure, but rather demonstrating decisive action to turn the group’s performance around.
The Pros to using an outside management firm are obvious. You are partnering with a firm that specializes in managing group practices. Beyond the on-site team, you have access to specialists who can respond with best practices to issues such as revenue cycle, front desk operations, patient flow and throughput, physician productivity and compensation, building the group culture, and identifying and nurturing physician leaders. Also using a firm that develops a strategic plan for the group will ensure that the goals of the group and the hospital are in sync. And the cost savings achieved by improved operations and avoiding costly missteps will, in most situations, cover the cost of the management fees.
