Ensuring the management team’s focus and capabilities match the scale and maturity of an employed physician network’s development is a challenge many healthcare systems face today. Many management teams get locked into a “doing things the way they’ve always been done” mentality, without acknowledging or accounting for the network’s evolving needs.
HSG’s Physician Network Growth Phases chart (pictured below) helps organizations revamp their capabilities to address the employed physician networks needs and ensure the network is progressing towards financial sustainability and value-creation for the health system.
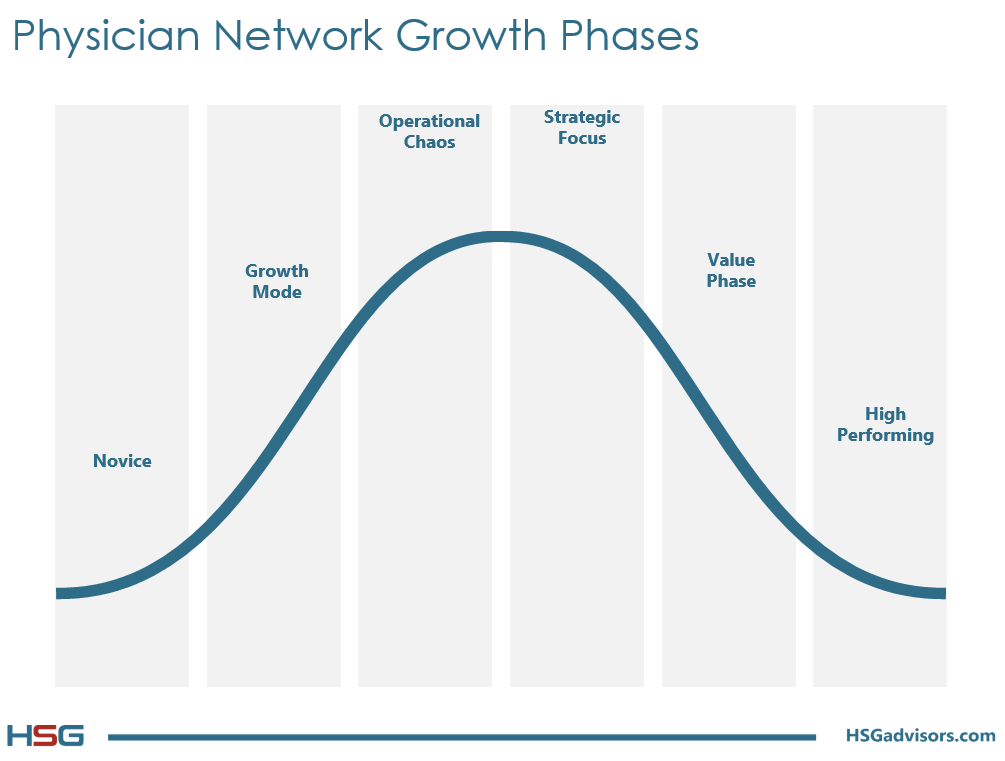
Below is an overview of each of the phases within the Physician Network Growth Phases, as well as challenges management teams will face in each phase, and supporting HSG-developed resources for tackling some of the challenges that are prevalent in each phase:
Stage: Novice
Description:
Novice organizations are dabbling in employment, mainly as a reactive measure, with no growth strategy. The network lacks a formal management infrastructure and can best be described as a group of independent physicians who share the same W2 form.
Key Current Challenges:
- Completing physician transactions given limited hospital executive bandwidth
- Defining the physicians who SHOULD be employed versus who is asking to be employed
- Developing basic management infrastructure to facilitate hospital management of physician practices
Stage: Growth Mode
Description:
Organizations in growth mode are beginning to aggregate in size, with some proactive physician employment based on perceptions of strategic need. Network remains loosely managed and is overseen by hospital execs juggling many other responsibilities in addition to the network.
Key Current Challenges:
- Selectivity about whom to employ
- Performing meaningful due diligence
- Thinking proactively about deal making and compensation to avoid future headaches
- Building a forum for physician leadership and engaging physicians about group growth
Stage: Operational Chaos
Description:
Network growth has outstripped the capabilities of those managing it. Increasing practice subsidies highlight the need for a formal, professional management infrastructure. Hospital leadership senses the need to control the group’s growth and limit employment offers.
Key Current Challenges:
- Acquiring the management talent the network needs to stabilize operations
- Building revenue cycle capabilities and systems into the infrastructure
- Developing a focus on management reporting, including a comprehensive dashboard
- Developing a Physician Advisory Council to lead the effort to develop a group practice approach and culture
Stage: Strategic Focus
Description:
Network operations are better aligned and the focus shifts to strategy. This is the time when the foundations for population management capabilities are laid. Weak/poor physicians who will not be successful in a value-based environment are culled from the group.
Key Current Challenges:
- Investing in best practices and reducing variation
- Ensuring appropriate referrals stay within the network
- Involving physicians in administration of group to drive clinical leadership
- Removing underperforming providers
- Tightening and building management capabilities
Stage: Value Phase
Description:
Network is more integrated and learning how to produce value from operational integration. The employed network is leading the charge to improve quality, serves as the core physician network for managed care offerings, and is the locus of the system’s efforts to control risk.
Key Current Challenges:
- Evolving compensation to address risk and quality incentives
- Defining provider productivity from a population management perspective
- Building information systems beyond managing the business to managing patient populations
- Integrating the group and system strategy into a clinical integration strategy
Stage: High-Performing
Description:
The network is stable in its growth and operations, and has developed both the culture and capability to manage populations and take on risk.
Key Current Challenges:
- Maintaining culture over time given physician turnover
- Physician leadership succession planning
- Integrating new IT tools into existing competencies around population management
