
|
Download a PDF Version to Share With Your Team |
Advanced Practice Provider (APP) collaboration presents a spectrum of physician involvement that varies according to experience level, specialty, APP productivity, and state and organizational review requirements. The effort required to fulfill these expectations should be distinguished and appropriately recognized in the physician compensation model.
Physician employment invokes regulatory parameters for compensation that do not exist in the independent, private practice environment – and therefore, may be a foreign concept to many physicians. In private practice settings, the collaborative effort associated with adding APPs to the care delivery team is a straight business case decision in which time and financial investments are offset by APP generated revenues – as long as individual physicians share in the practice’s net patient care revenues. For employed physicians, the Stark laws and regulations permit health systems to compensate physicians for “personally performed” services, which are commonly based on or equated to the wRVUs generated through individual, personally rendered professional services. Conversely, the Stark laws and regulations prohibit health systems from compensating physicians for services that were not personally performed – such as services performed by APPs without direct or sufficient physician involvement. Therefore, the private practice model of sharing in APP generated net revenue risks noncompliance with the legal parameters imposed on hospital and health system employed physician compensation models.
Since the private practice APP collaboration compensation model cannot be directly applied to employed networks, innovative approaches must be considered. Nationally, Sullivan Cotter respondents indicated that 56% offer additional compensation to physicians for supervising APPs1 and IHS respondents indicated that 72% offer additional compensation to physicians for supervising APPs.2 Both surveyors indicated that the most common approach is through a fixed stipend for APP collaboration/supervision. The fixed stipend recognizes responsibilities associated with fulfilling collaboration requirements and allays compliance concerns related to “personally performed” services parameters.
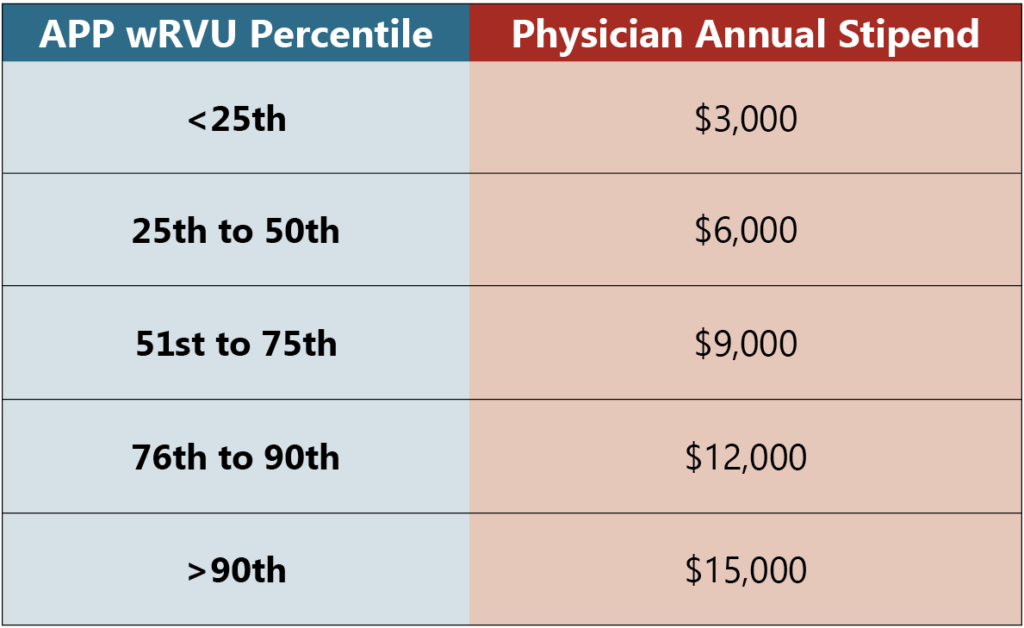
Addressing the varying levels of effort required by differing collaboration circumstances adds complexity to compensation models but is overwhelmingly well received. For instance, the additional physician effort expended during collaboration with very busy APPs compared to less busy APPs can be recognized by linking fixed stipend amounts to APP productivity. This tiered approach acknowledges that more productive APPs generate more daily interactions, greater periodic care review requirements (when based on % of APP encounters), and correspondingly greater levels of effort. IHS respondents were more likely than the Sullivan Cotter respondents to include incentives tied to APP productivity (55%).1,2 The following illustrates a sample tiered stipend approach based on APP productivity:
Another instance considers the level of effort related to collaboration with new APP graduates compared to experienced APPs. This situation can be recognized by an increased fixed stipend during the first 6-12 months of mentoring with stepwise decreases to the base rate. An example of this approach might be to grant a $15,000 stipend for the first three months (> 90th percentile1) then decreasing to $12,500 (slightly > 75th percentile1) for six months then to the median of $10,000 (median1) thereafter – with corresponding decreasing collaboration expectations over the same time period (see the following example).
If a fixed stipend approach is pursued, mechanisms to define associated expectations and to regularly monitor compliance with them must also be implemented. One approach is to establish local APP Collaboration Agreements that delineate expected physician responsibilities, such as providing daily availability for timely mentoring and feedback, designating definitive coverage during absences, periodically reviewing clinical and prescribing protocols, and reviewing an explicit number or percentage of APP encounter documents at specified intervals. Separate sections of the agreement could address mentoring new graduates versus collaborating with established APPs, with each section outlining respective required actions. Linking to the new graduate collaboration stipend example above, requirements for the first three months might include daily chart review with direct APP feedback for the first 2 weeks followed by weekly chart review of 20% of encounters for 4 weeks followed by weekly review of 10% of encounters for 6 weeks with submission of the reviews to the Quality Coordinator as part of the Initial Professional Performance Evaluation process. Monitoring could include verification that the reviews are completed and submitted as required and periodic “how are things going” interviews with the APP to ensure that direct feedback occurred. The next 6-month interval could require a 10% monthly review and submission process leading to the “base” 10% quarterly record review and submission thereafter to support the Ongoing Professional Performance Evaluation process.
Matching physician compensation incentives with APP collaboration expectations overcomes a potential barrier to APP utilization and aligns physician efforts with the organizational benefits associated with APP assimilation in care delivery models. HSG would welcome the opportunity to discuss this and other issues related to either APP utilization or physician and APP compensation.
Cited References
Please let us know if we can be of any assistance with developing and implementing APP oversight and collaboration in your physician compensation models by contacting Dr. Terry McWilliams or Neal Barker directly.
- Sullivan, Cotter, and Associates (“SC”) 2019 Physician Compensation and Productivity Survey Report.
- Integrated Healthcare Strategies (“IHS”) 2018 Physician Compensation and Production Survey, Compensation Survey Report.

