|
Download a PDF Version of the Article to Share With Your Team |
2021 Medicare Physician Fee Schedule Final Rule: A Catalyst for Comprehensive Compensation Redesign
The 2021 Medicare Physician Fee Schedule (“MPFS”) Final Rule is a significant milestone that recognizes the increased administrative burden placed on today’s direct care providers when rendering patient care. The 2021 MPFS can also create an opportunity for health systems to shift their compensation philosophy and structures to be less dependent on volume and more prominently recognize value. This shift will more closely align provider incentives and payer reimbursement, and promote greater long-term financial sustainability of health care organizations. Many health care organizations talk about the need to move towards value, but few walk the walk as they procrastinate based on current health care dynamics or day-to-day workload…or fears of upsetting the current applecart. While the move to value-based reimbursement, and its level of maturity, varies by market, we believe that the move is imminent for previously untouched markets. Since health systems are going to have to eventually address this shift to value, HSG believes now is a good time as the 2021 MPFS Final Rule can serve as a perfect catalyst for change.
Although the Consolidated Appropriations Act (signed into law on December 27, 2020) ultimately lessened the degree of adverse financial impact related to the decreased conversion factor (3.4% decrease instead of 10.2% decrease), the 2021 MPFS will still create significant issues related to:
- Individual provider coding curves due to the revised coding documentation requirements for E/M codes 99202-99205, 99211-99215 and the elimination of 99201. The impact of this rather select action will clearly vary by specialty. There will be less financial pressures than originally estimated but still some depending on group type and service mix (primary care vs. specialty care vs. medical specialty vs. E/Mheavy vs. procedural service-heavy).
- Level of wRVU credit afforded to E/M codes 99202-99205, 99211-99215 and many other E/M codes, CPT codes, and associated bundles. The impact of these changes also varies by specialty, with “cognitive” specialties benefiting more greatly than “procedural” specialties.
- Actual Medicare reimbursement.
Analysis is needed on a case-by-case basis in order to fully understand the compensation and reimbursement impact organization to organization.
Since release of the Final Rule in early December 2020, HSG has been working with clients to vet the three major variables (coding documentation changes, compensation impact, and reimbursement projections), predict the collective impact on the future of health systems, and develop a plan for addressing provider compensation within the organization.
IMPORTANT STEPS TO ADDRESSING PROVIDER COMPENSATION AS A RESULT OF THE 2021 MEDICARE PHYSICIAN FEE SCHEDULE FINAL RULE
- Coding − It is critical to evaluate the change in coding patterns over the first six months of 2021, how those changes compared to historic performance, and what impact the difference will have on compensation and reimbursement.
- Compensation − Primary care vs. specialty care compensation structures. With increases in E/M wRVU values and a decrease in the Medicare conversion factor, ultimately, someone has to win, and someone has to lose in productivity driven compensation models. Compensation for primary care and many non-procedural medical specialty care providers will most likely increase while procedure-based specialty care provider compensation will most likely decrease – or need to become more quality/outcome focused. Organizations will need to decide if procedure-based specialists are going to be kept “whole.” If so, how? Where does the money come from?
- Value-based Reimbursement − Reimbursement for health care services is progressively shifting more aggressively to a value-based environment. Bundled payment initiatives and value-based reimbursement need to be addressed to avoid leaving current, and future, revenue opportunities on the table.
HOW TO ADDRESS EACH COMPONENT
- Coding − Provider educational sessions including:
- Overview of 2021 MPFS Final Rule
- New E/M coding documentation requirements
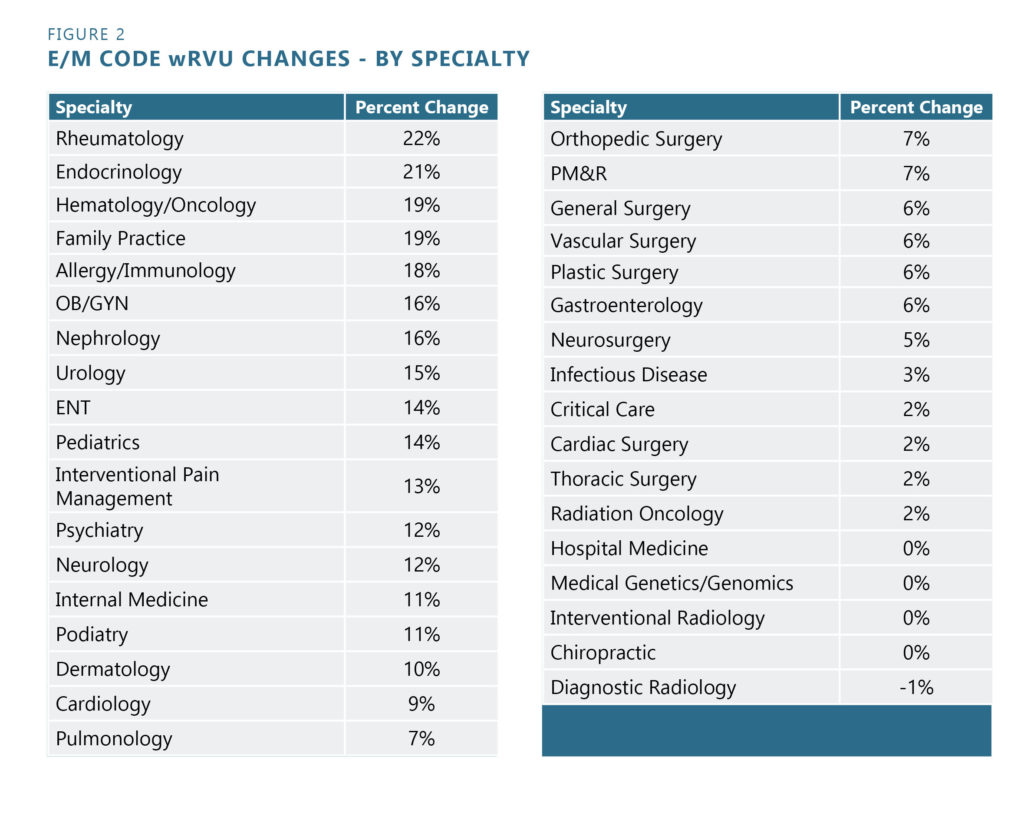
- Potential impact of wRVU changes (see Figure 1)
- Potential impact to organizational revenue
- Discussion of wRVU and compensation impact by specialty (see Figure 2)
- Discussion on changes to compensation rates in the future
- Monitoring, measuring, and providing direct feedback of actual versus potential impact in all of these areas
- Compensation
- Baseline analysis of current relationship between compensation and productivity
- Determine accurate baseline level of historic performance
- Create baseline volume projections by specialty for 2021 and beyond
- Estimate potential wRVU impact based on 2021 Medicare Physician Fee Schedule changes and coding scenarios
- Evaluate contractual latitude to defer the immediate impact until the predicted impact can become validated or refuted
- Long-term impact analysis
- Analyze E/M coding distribution and project full impact of 2021 Medicare Physician Fee Schedule Final Rule on 2021 volume and coding trends by specialty
- Recommend rate adjustments that are sustainable for the health system long-term
- Decide philosophy and position regarding providers that “win” and providers that “lose” or if every provider should be kept “whole” in the future
- Baseline analysis of current relationship between compensation and productivity
- Value-based Reimbursement − Reimbursement for health care services is progressively shifting more aggressively to a value-based environment. Bundled payment initiatives and value-based reimbursement need to be addressed to avoid leaving current, and future, revenue opportunities on the table.
- Baseline analysis of current relationship among productivity, compensation, and reimbursement
- Create baseline reimbursement projections by specialty for 2021 and beyond created by the decreased conversion factor.
- Estimate potential reimbursement impact based on shifts in provider productivity (altered coding curves and wRVU credits) and compensation dynamics (production vs. non-productivity breakdown).
- Determine current level of pay-for-performance incentives associated with current federal and commercial payer contracts – and measure system performance against those metrics.
- Long-term impact analysis
- Analyze E/M coding distribution and project full impact of 2021 MPFS Final Rule on 2021 volume and reimbursement impact by specialty.
- Note the anticipated lost revenue due to underperformance against pay-forperformance incentives.
- Determine mechanisms to incorporate non-productivity incentives into the compensation models to align provider and organizational reimbursement incentives.
- Baseline analysis of current relationship among productivity, compensation, and reimbursement
Change is never easy. However, undertaking simultaneous changes in three major interdependent variables that affect provider compensation and organizational reimbursement is a significant challenge with which absolute impact is difficult to predict. Temporizing measures that maintain 2020 compensation variables through 2021 will allow determination of the actual impact of these changes over the first 6-9 months of 2021 leading to a comprehensive re-assessment and revision of provider compensation models heading into 2022. HSG can assist with these processes and permit networks to emerge from 2021 having addressed the 2021 Medicare Physician Fee Schedule Final Rule and preparing more concretely for the future of value-based care and reimbursement.
Figure 1
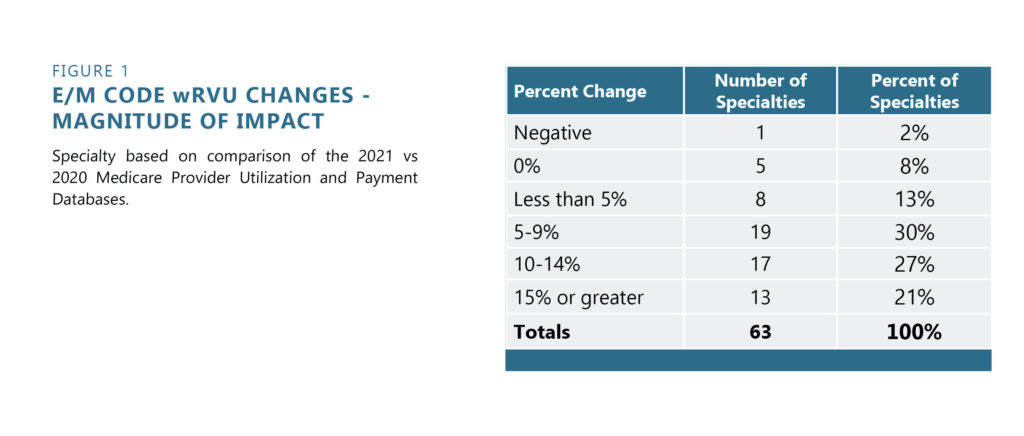
Figure 2