Authors:
Neal D. Barker, Partner
Dr. Terry McWilliams, Chief Clinical Officer
Read or download the article as a PDF, or read below:
As you now undoubtedly now know, CMS changed coding and documentation requirements for many E/M encounters with the 2023 Medicare Physician Fee Schedule Final Rule. These changes became effective January 1st, 2023, and applied the office-based coding documentation changes promulgated in the 2021 Medicare Physician Fee Schedule Final Rule to the “other” E/M encounters and streamlined the coding process for many clinical encounters.
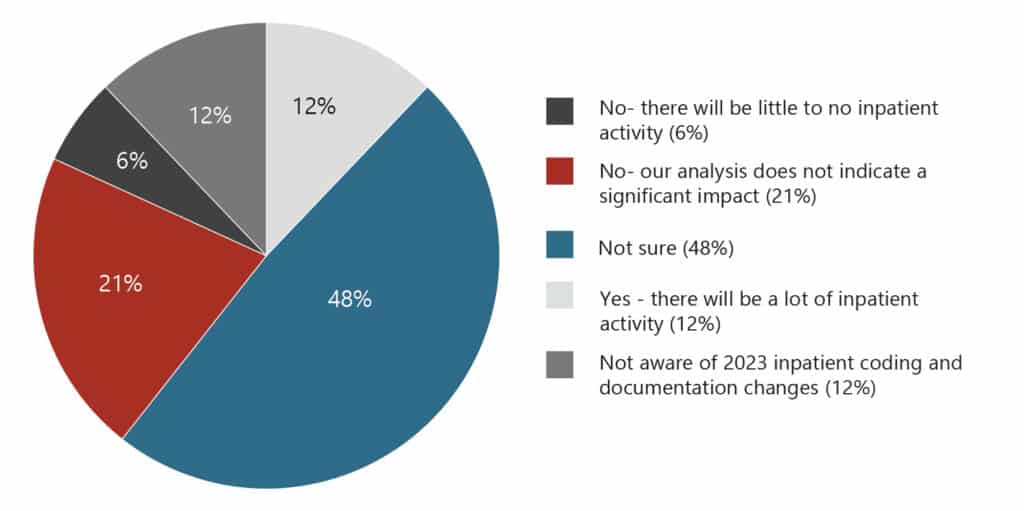
In January, HSG conducted a survey about several provider compensation topics – including how organizations perceived the new coding and documentation changes would impact them. Considering the survey occurred shortly after the changes became effective, many respondents (48%) were unsurprisingly not sure how the changes would impact them – 12% did not even know what the changes involved. Of those that had formed an opinion, 12% thought the changes would have a significant impact on their organization while 21% thought the changes would not.
FIGURE 1:
Do you think the 2023 inpatient coding and documentation changes will impact your providers’ coding curves and compensation?
Now that everyone has had a few months of actual experience with the changes, we wonder how folks are faring. To that end, this article will review the changes so that we have a common frame of reference, then frankly ask how things are going for you all. We will start with reviewing the coding documentation changes, then progress through the actual coding changes.
2023 E/M CODING DOCUMENTATION CHANGES
1. What are the 2023 E/M Coding Documentation changes?
An effective policy should clearly define roles and responsibilities while establishing the specific parameters and expectations for the APP Oversight Program and apply them across the entire organization.
As noted above, CMS applied the coding and documentation changes promulgated in the 2021 Medicare Physician Fee Schedule Final Rule for office-based E/M encounters to the “other” E/M encounters. Through this action, CMS created a unified set of coding documentation rules for all E/M encounters regardless of the location of care – and took a leap forward in their ongoing intent to decrease the administrative burden associated with the encounter coding process.
Providers now determine the coding level for any E/M encounter by using either a modified medical decision-making (MDM) approach or a total time dedicated (Time) approach – with some notable exceptions. Only the MDM approach applies to Emergency Department encounters and Cognitive Impairment Assessments. Conversely, only Time approach applies to critical care encounters and hospital discharges.
Coding levels are no longer determined by the extent of the history and examination. In contradistinction to the 1995 and 1997 coding criteria, only a history and physical examination that is “medically appropriate” for the issue being addressed/ evaluated is the new guidance.
What encounters do the new coding documentation changes apply to?
2. What encounters do the new coding documentation changes apply to?
The 2023 coding documentation applies to the following “other” E/M encounters:
-
- Hospital inpatient and observation status patient encounters
- Emergency Department patient encounters
- Nursing Facility patient encounters
- Home/residence services patient encounters
- Cognitive Impairment Assessments
3. What does the modified medical decision-making (MDM) coding documentation approach involve?
The MDM methodology involves four (4) levels of medical decision-making – straightforward, low, moderate, and high–based on consideration of the following three (3) factors:
-
- Number and complexity of problems addressed (“problems”)
- Amount and complexity of data reviewed/considered (“data”)
- Patient risk of complications/morbidity/mortality (“risk”)
The level of E/M service selected is that which is satisfied by at least two (2) of these three (3) elements (problems, data, risk).
The highest-level code automatically results when any of the following situations apply:
-
- Escalating care (e.g., transfer to ICU)
- Deescalating care or discussing DNR status due to poor prognosis
- Initiating medications that require intensive or invasive monitoring
- Deciding on emergency surgery regardless of patient risk factors
Since the MDM approach is very similar to the 2021 office-based requirements, it results in comparable crossovers related to complexity. Under the new changes, the following pattern emerges:
-
- Level 1 initial or subsequent hospital visit criteria = level 3 office visit
- Level 2 initial or subsequent hospital visit criteria = level 4 office visit
- Level 3 initial or subsequent hospital visit criteria = level 5 office visit
Summary crosswalks of criteria for “problems,” “data,” and “risk” across clinical settings exist. An easy-to-use reference is available through the American Society of Clinical Oncology website.(1)
4. What does the total dedicated time (Time) coding documentation approach involve?
The Time methodology accounts for all personally dedicated time the billing provider spent caring for the patient before, during, and after the face-to-face encounter(s) on the day of service. The criteria are the same as for the office-based encounter and the dedicated time includes medical record and results review, encounter documentation, additional consultations, or care discussions with colleagues, and talking with family or caregivers in addition to the time spent in the actual face-to-face patient encounter. The time accrual does not apply to time spent traveling to and from locations of care, time spent in formal teaching endeavors, or time spent performing separately billable procedures. Time dedicated to a patient admission that extends beyond midnight can be included in the day of admission time frame (part of the previous day) as it applies to a single patient encounter that crossed into the next day.
Summary crosswalks of criteria for dedicated time spent across clinical settings exist. An easy-to-use reference is available from K. Millette, MD, “The 2023 Hospital and Nursing Home E/M Visit Coding Changes.” FPM, January/February 2023. https://www.aafp.org/pubs/fpm/issues/2023/0100/hospital-em-coding.html
5. What impacts have the 2023 coding documentation changes had?
On the surface, and in CMS’ opinion, the impact of the changes depends on historic individual coding curves and whether providers continue to use MDM or use Time. If providers use the MDM approach, very little impact is expected. However, coding levels may increase if using Time offers an advantage.
-
- Have providers continued to use the familiar MDM approach – or have they moved to time spent when advantageous?
- Capturing and documenting time spent is a foreign concept for many specialties. Have the providers devised mechanisms to accurately accomplish this change?
- Historic EMR documentation templates were designed to capture elements of the history and physical and have not focused on the criteria applicable to either of these coding documentation approaches. How have you, or your vendor, revised documentation templates to accurately capture information to maximize coding potential? Are you capturing the thought processes behind the plan of care development?
- Have individual and group coding curves, wRVU generation, or reimbursements changed because of the 2023 coding documentation changes?
2023 E/M CODING CHANGES
CMS’ intent to decrease the administrative burden of the coding process really came to the fore with the E/M coding changes promulgated in the 2023 Medicare Physician Fee Schedule Final Rule. We will focus on some of the most impactful changes.
1. Observation Status
Observation status no longer exists. CMS eliminated observation status codes 99217-99220 and 99224-99226 and merged these patients into the existing hospital care codes – and modified the definitions accordingly – as follows:
-
- 99221-99223 – Initial inpatient or observation care per calendar day … 40, 55, and 75 minutes must be met or exceeded respectively
- 99231-99233 – Subsequent inpatient or observation care per calendar day … 25, 35, and 50 minutes must be met or exceeded respectively
- 99238-99239 – Hospital discharge day management … < 30 minutes or greater than 30 minutes respectively
These changes make administrative processes from patient registration to claims submission more seamless and less confusing or confounding for all involved – especially patients.
CMS did retain CPT codes 99234-99236 … Admission and Discharge on the same day – either inpatient or
observation – for which 45, 70, and 85 minutes must be met or exceeded respectively
2. Inpatient Care
CMS modified the definitions of initial and subsequent care as follows:
-
- Initial – When the patient has not received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the same specialty who belongs to the same group practice during the stay.
- Subsequent – When the patient has received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the same specialty who belongs to the same group practice during the stay.
This addresses a longstanding provider complaint related to the lack of recognition of the complexities of cross-coverage and may allow for greater reimbursement and wRVU accrual in instances of cross-coverage by different groups of the same specialty during a hospital stay. Members of different same-specialty groups seeing patients for the first time during a stay can now bill for initial rather than subsequent day care.
3. Consultation Services
CMS deleted the lowest level office (99241) and inpatient (99251) consultation codes, which aligns with the four levels of medical decision-making (Office 99242-99245) (Inpatient/Observation 99252-99255) – and is consistent with the elimination of the office E/M code 99201 in the 2021 Medicare Physician Fee Schedule Final Rule (New Patient 99202-99205). These changes should really have negligible reimbursement and compensation impact – but do streamline options.
4. Emergency Department Services
CMS redesignated the lowest ED level code (99281) to visits that do not require physician or APP involvement – much like the office-based code 99211. This change should also have negligible reimbursement and compensation impact.
5. Nursing Facility Services
CMS adopted the same definitions for initial and subsequent care in nursing facilities as it did for inpatient/ observation care outlined above. This change will likely have less impact in this environment of care than in the hospital.
CMS also eliminated the code for the annual nursing facility assessment (99318). This care is now reported through the subsequent care codes (99307-99310). Code comparisons indicate that this change will have only a marginal impact on reimbursement and compensation.
6. Home and Residence Services
CMS deleted domiciliary or rest home codes (New Patient 99324-99328; Established Patient 99334-99337) and merged the care with existing home visit codes 99341-99350 (New patient 99341-99345; Established patient 99347-99350) … and deleted 99339, 99340, and 99343. These changes at least reduce coding complexity by combining “home-based” encounters in a single category.
7. What impact have the 2023 coding changes had?
Obviously, the actual impact will depend on individual scopes of care – but they are not predicted to have a major impact on reimbursement or compensation. The changes should, however, streamline processes and decrease complexities. Has this been your experience?
The 2023 Medicare Physician Fee Schedule Final Rule changes are delineated in greater detail in the January 31st AAPCP webinar captured on HSG’s website at 2023 Medicare Physician Fee Schedule l HSG Advisors.