Co-written by: Dr. Terrence McWilliams, MD, MSJ, FAAFP and Lesli R. Lair, RHIT, CPC, CRC, CPMA
OVERVIEW
Accurate, complete encounter documentation and appropriate encounter coding are fundamental elements of a comprehensive Professional Services Coding and Documentation Audit and Education Program.
Developing, implementing, and executing a program of this complexity can be a daunting undertaking, but the reward of maximizing and positively impacting patient care revenue, provider productivity, financial sustainability, and corporate compliance is well worth the effort.
Read below to learn which elements of a program HSG’s coding and documentation experts find most important, and how they can be applied to your teams.
PROGRAM COMPONENTS
There are several foundational components to consider when developing your comprehensive program:
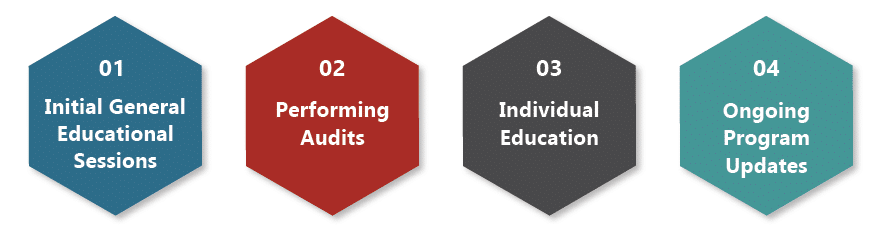

1. INITIAL GENERAL EDUCATION SESSION
An initial education session when starting the program is needed for new providers who code their own patient encounters should be a standard part of the onboarding process. Many practicing providers have a limited understanding of professional services coding processes because, historically, they received limited training on this crucial topic during their education and training programs. Even as some training programs are now incorporating more coding education, competing priorities and a lack of immediate applicability and direct feedback hinder the impact of these efforts.
Completing a general educational session when the program is initiated and during new provider onboarding helps to impart a basic understanding of the coding and documentation criteria, ensuring at least a baseline understanding of the 2021/2023 criteria and processes. These sessions create a common mental model and emphasize the importance of the coding process, establishing a firm foundation for future documentation and coding interactions.

2. PERFORMING AUDITS
Chart audits need to be performed to compare encounter documentation with the corresponding ICD-10 and CPT code selection on submitted claims. The documentation must fully support the assigned CPT, HCPCS, and ICD-10 codes for the encounter.
- The initial audit tends to review a greater number of encounters and should ideally include at least a small sample from each relevant area of the provider’s scope of practice and visit types, including procedures, to offer a comprehensive overview of coding performance. Providers who practice in both the inpatient and outpatient environments should have encounters sampled in each area. Other potential target areas include encounters associated with modifiers or bundling/unbundling.
- Subsequent audits tend to review a lesser number of encounters and could target specific practice areas, appointment types, or areas initially identified as having the greatest opportunity for improvement. This approach allows for more extensive sampling and offers a more in-depth educational experience.
Provider coding programs historically focused on the proper selection of CPT (E/M, procedural, and HCPCS) codes, as these tended to be the primary determinants for payer reimbursements and provider productivity – and therefore, compliance risk. The shift from the 1995 and 1997 coding and documentation guidelines to the revised coding and documentation guidelines promulgated by the 2021 (outpatient) and 2023 (inpatient, SNF) Medicare Physician Fee Schedule Final Rules heightened the importance of ensuring the highest specificity ICD-10 codes are selected to most accurately depict patient complexity.
Patient complexity plays an important role in medical necessity justification and in medical decision-making difficulty, and the most appropriate level of E/M code selection- regardless of whether dedicated time spent or medical decision-making criteria are used. Utilizing the proper ICD-10 codes to accurately and specifically capture the patient’s conditions is receiving greater attention due to its impact on determining the most appropriate level of E/M code selection under the current coding and documentation rules – regardless of whether dedicated time spent or medical decision-making criteria are used.
- When using the dedicated time spent pathway, accurately representing the patient’s level of complexity justifies the time dedicated to the patient’s care on the day of service.
- When using the medical decision-making pathway, accurately depicting the patient’s level of complexity plays a significant role in indicating the complexity of problems considered; justifying pertinent orders entered, data reviewed, and medications managed; and ultimately contributing to patient outcome risk.
Beyond E/M code selection, utilizing the proper ICD-10 codes to accurately and specifically capture the patient’s conditions contributes to defining patient complexity measured by Hierarchical Condition Category (HCC )scoring and Risk Adjustment Factors (RAFs). These are calculated in large part by ICD-10 code designations on submitted claims – which in turn are used to determine Medicare Advantage plan reimbursements. An additional benefit of accurately depicting patient complexity, up until this year, was the opportunity to qualify for bonus points in the Quality Payment Program’s MIPS pathway scoring. Since using non-specific or unspecified condition codes can lead to woefully under-appreciated patient complexity, the increased importance of proper ICD-10 code selection has elevated its status as a key component of coding audit programs.
As previously stated, CPT codes (E/M, procedural, and HCPCS) historically received the greatest attention in coding and documentation audits, as these form the basis for revenue generation and productivity determinations. E/M codes are determined by patient interaction complexity based on the medical record documentation. The documentation must reflect the level of effort expended and the degree of complexity reported. CPT procedural codes (and HCPCS codes) are generally more straightforward but their accuracy also depends on precise, complete encounter documentation.
Equally important is the correct application of modifiers across all CPT codes. Although often misunderstood by providers, inexperienced revenue cycle staff, and even coders, modifiers play a critical role in coding accuracy, appropriate reimbursement, and wRVU attribution. Improperly applying a modifier or omitting the correct modifier can lead to unnecessary denials or incorrect reimbursement. Additionally, failing to account for modifiers in the wRVU attribution process is a common pitfall when assessing provider productivity, often resulting in excessive credit being granted.
A comprehensive coding and documentation program should extend the historic reach of coding audits to impart insights regarding the impact of the suggested coding changes on wRVU attribution and organizational revenues. This facet of the program calculates the differences in attributed wRVUs between the original, provider-selected CPT codes and the auditor-suggested CPT codes, which then informs the impact on resultant provider productivity credit and compensation. This facet of the program also predicts the impact of the suggested coding changes on organizational revenues using the national CMS maximal allowable charges benchmarks. These additional determinations allow the organization to more completely understand the potential positive and negative financial impact of the suggested coding changes.

3. INDIVIDUAL EDUCATION
Adult learning theory predicts that general educational sessions which are not directly linked to daily experiences tend to yield incomplete and transient retention of the information – even when reference materials are provided. (This explains in part why some of the training programs, mentioned earlier, are not as impactful as on-the-job education.)
The most reliably lasting impact is realized with frequent, critical review of individual performance with timely, specific 1:1 individual feedback and education with practical, actionable suggested interventions. Reported observations and recommendations span all aspects of the audit – ICD-10 code selection, CPT code selection, and documentation improvement suggestions. These educational performance feedback sessions delve into and emphasize specialty-specific elements involved in the coding and documentation process.

4. ONGOING UPDATES
Scheduling follow-up audits along with individual educational feedback sessions reinforces previous recommendations and invariably uncovers new territories to discuss. The frequency of follow-up audits tends to depend on the degree of individual improvement opportunities and the receptiveness of the individual and the organization but undertaking an audit and feedback cadence of every 3-6 months is common.
PROGRAM IMPACT
Maximizing professional services coding and documentation performance improvement directly impacts several key areas:
Patient Care Revenue
- Appropriately coding patient care encounters accurately captures direct patient care efforts and directly determines network revenues related to these efforts. Under-coding leads to receiving less reimbursement than the provider/organization is entitled to for the level of effort expended. In other words, under-coding leaves money on the table.
- Accurately coding patient encounters also impacts the determination of HCC status, which, among other uses, factors into performance scoring for the MIPS path of the CMS Quality Payment Program and per member per month payments in capitated environments. Under-coding underreports patient complexity and adversely impacts the HCC.
- Coding accuracy can also impact health insurer-driven, claim-based pay-for-performance programs and capture of at-risk reimbursement monies.
Productivity Measurement
- Coding levels – along with the appropriate use of modifiers – are directly tied to wRVU calculations, which form the foundation of many provider productivity models. Since coding-generated wRVU credit is the cornerstone of commonly utilized provider compensation models, coding accuracy directly impacts provider compensation – an issue that impacts both network administrators and providers.
- Additionally, individual wRVU levels and associated specialty-specific performance percentiles provide objective measures that drive capacity determinations for network performance improvement initiatives and recruitment prioritizations.
Corporate Compliance
- Ensuring coding accuracy protects organizations from erroneous claims submissions and resulting reimbursements. The primary compliance risk involves provider over-coding leading to overpayment and recoupment/restitution scenarios. Improper use of modifiers also increases compliance risk by leading to unbundling or creating misleading representations of services. When discovered, dilemmas arise related to self-disclosure versus discovery (think whistleblower) and associated False Claims Act implications. Regular audits mitigate this risk as part of organizational due diligence.
- Another compliance risk is related to wRVU-based provider compensation: Providers are ultimately responsible for the code assigned to each patient encounter. When providers self-code patient encounters, they could hypothetically upcode to their own inurement. Since wRVU calculations are based on encounter coding and higher levels of E/M codes result in higher levels of wRVUs, provider upcoding or over-coding can result in additional/excessive compensation for providers. This assertion does not presume that any provider would intentionally over-code to his/her own benefit, but it is incumbent on organizations to ensure that checks and balances are in place to avoid any perceived or actual impropriety. Regular audits mitigate this risk as part of organizational due diligence.
- Some organizations perform compliance audits once a year on a small sample of encounters, often ten (10). While this level of review might satisfy corporate compliance requirements, it is inadequate to impact coding proficiency. A more robust program fulfills both aspects – coding and documentation improvement and corporate compliance.
Coding and Billing Process
- Implementing and executing a comprehensive coding and documentation audit and education program invariably produces incidental benefits related to observations and insights about the organization’s coding and billing processes that permit secondary performance improvement initiatives.
CONCLUSION
Maximizing coding and documentation accuracy has historically been undervalued and under-supported in many employed provider networks. The impact – both positive and negative – can no longer be ignored. We must embrace this aspect of practice operations as a critical sustainability issue and pursue corresponding investments pursued.
When you’re ready to evaluate your organization’s coding and documentation programs, reach out to Terrence R. McWilliams to get started.
