Considerations for Medical Staff Call Coverage Compensation
Author: Neal Barker, Partner and Managing Director, Compensation and Compliance
Historically, as part of their responsibilities as members of the hospital’s medical staff, specialists have provided emergency department call coverage and consulted on patients admitted through the emergency department, doing so without incremental compensation. Not only was taking call something everyone on the medical staff did as a shared duty, it was also a way to build one’s practice- indirectly impacting compensation.
Today, the thought of uncompensated call coverage seems to be relic from a bygone era. There are several reasons this could be, whether due to an employee-employer mindset that we’ve seen emerge as more and more physicians sell their practices to hospitals and become hospital/health system-employed physicians, or because newer physicians exit training seeking an employed situation. It could also be due to the proliferation of ambulatory surgery centers (ASCs) and surgical care advancements that allow more and more surgeries and procedures to be performed in an ASC or office, meaning physicians don’t need hospitals in the same way they used to. Or, driven by a decline in reimbursement, coupled with increasing practice overhead and costs and independent physicians’ need to focus on the most profitable services. Whatever the reasons, the hospitals’ and health systems’ struggle to maintain needed call coverage escalates year after year.
Hospitals need specialists’ call coverage to provide safe, efficient, and comprehensive care. Hospitals also need specialists’ call coverage for compliance with legal requirements that apply to emergency departments. The Emergency Medical Treatment and Labor Act (“EMTALA”) of 1986 requires hospitals with emergency departments to provide a medical screening examination to any individual who comes to the emergency department and requests such an examination and prohibits hospitals with emergency departments from refusing to examine or treat individuals with an emergency medical condition.

EMTALA also requires that hospitals with dedicated emergency departments, “maintain a list of physicians who are on-call to provide further evaluation and or treatment necessary to stabilize an individual with an emergency medical condition.”(1) Unfortunately, many hospitals and health systems are only reactive to the question of call pay, rather than proactive.
Often it seems as if hospitals don’t want to think about call pay—if they don’t bring it up, perhaps no one on their medical staff will either. Frequently, they discover that “hope” is not a strategy and having their head down doesn’t work. We are not suggesting that hospitals should run to the specialists on their medical staff and ask them if they would like to be paid for call- that is NOT the sort of proactive step we are talking about here. Rather, a hospital’s medical staff bylaws should first and foremost require a minimum number of days of call per month per physician in a specialty’s call rotation. This minimum number of days must be satisfied before call pay can even be considered—unless a particular specialty’s situation demonstrates that pay for each day of call is necessary.
Buckhead FMV’s 2023 Physician Call Coverage Burden and Compensation Survey2 provides data, by specialty, regarding the number of compensated versus uncompensated days per month. Based on that data and focusing on the median to 75th percentile, we calculated an average of 7-to-10 days per month (median to 75th percentile) that are uncompensated across twenty-six (26) specialties for which sufficient data was reported in Buckhead FMV’s survey. The survey’s uncompensated days median ranged from a high of fifteen (15) days to a low of three (3) days and the 75th percentile ranged from a high of thirty (30) days to a low of 6.5 days. To participate in Buckhead FMV’s 2024 Physician Call Coverage Burden and Compensation Survey, please visit the following link: https://www.surveymonkey.com/r/F2QDJQL.
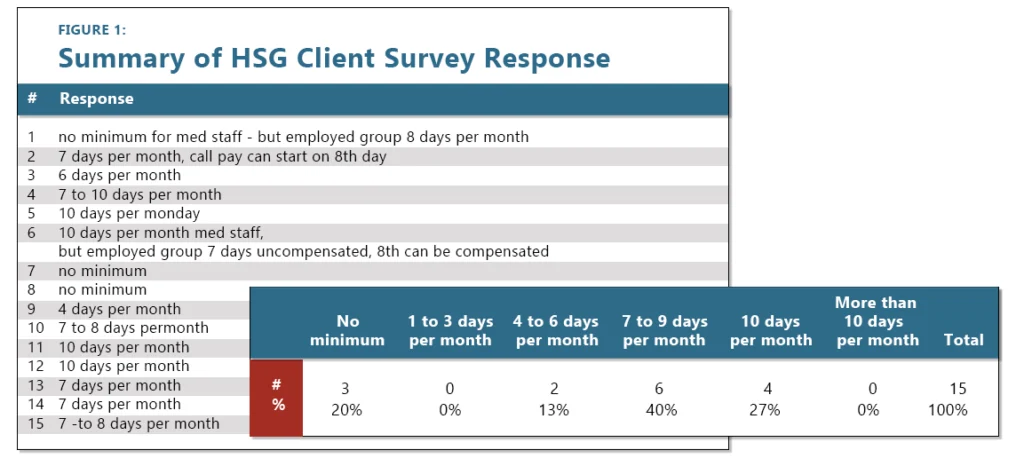
Additionally, on a much smaller scale, HSG surveyed fifteen (15) clients regarding their organization’s medical staff standard as it pertains to compensated versus uncompensated call days. The results of HSG’s mini survey reflected the results of Buckhead FMV’s comprehensive survey, again 7 to 10 days per month uncompensated was a common response.
Beyond maintaining a standard regarding the number of required uncompensated days of call per month per physician, hospitals should have a standard process for evaluating the need for call pay, as well as a methodology for assessing the burden of call for a particular rotation and ensuring that the relative burden of call is factored into the call rate (per diem) determination. This can be completed by an outside fair market value/commercial reasonableness vendor, or internally by the hospital/health system.
Either way, the following highlights some, but not all, of the questions that should be asked during a call pay evaluation process. The answers to these questions are central to the evaluation of the need for call, as well as the determination of the most appropriate rate based on the burden of call.
1. What is the specialty/service being covered?
Total compensation and compensation expectations are different from specialty-to-specialty. An amount that might motivate a primary care physician to take a call shift, may not motivate a neurosurgeon. Additionally, each specialty has its own inherent expectation of call burden. In other words, with some specialties, call comes with the territory; in other specialties, not as much. For example, if you practice in orthopedic surgery, your expectation of call coverage should be higher than a nephrologist or a dermatologist.
2. Is the physician providing on-call coverage at multiple facilities concurrently? If so, how many facilities is the physician providing on-call coverage for concurrently?
Concurrent coverage makes a difference because of patient volume and the increased likelihood of response. Just because I’m covering three (3) facilities concurrently doesn’t mean I am justified in receiving three (3) times a fair market value daily rate as call compensation. Call compensation data is per rotation, not necessarily just per facility. If the volume for my three (3) facility rotation is low and I am rarely called and infrequently must come into the hospital, then I may not be justified for a full single rate, much less a rate times three (3). Conversely, if the volume from my three (3) facilities is so significant that a second or third physician is normally required to respond as well because I’m busy with the first call, then the call money needs to be allocated to the other physicians.
3. Addressing the presence of provider-based billing in employed network offices.
Provider-based billing necessitates compliance with “hospital outpatient department” designation requirements for the involved practices. These requirements include specific licensure requirements, clinical services and reporting structure integration, financial accounting methodologies, and others. It’s possible that a health system may need to become a licensed entity with consolidated Boards, Medical Staffs (and Bylaws), and reporting structures reflecting and truly functioning in that fashion in order to manage and maintain compliance. Legal counsel guidance regarding this complicating factor is imperative.
4. How may physicians are in the on-call rotation per facility?
Clearly, the number of physicians in the rotation is critical, as this determines how frequently each physician is the on-call physician for the day. Based on the Buckhead FMV data previously presented and HSG’s client survey, we’ve said that seven (7) to ten (10) days per month of uncompensated call (or required uncompensated days per medical staff policy), is typical. Assuming this is accurate, a standard call rotation cutting across all specialties would have approximately four (4) physicians. Obviously, as the Buckhead FMV data shows, this may vary by specialty; specialties with a higher burden of call may need more physicians in the rotation for it to be manageable, given the daily patient volume, and/or they may be justified in being paid for each day of call.
5. Will the physician(s) be paid for each day of call or only extra call after days required by medical staff bylaws?
The Office of Inspector General’s September 20, 2007 OIG Advisory Opinion No. 07-103 describes a favorable opinion of an arrangement in which on-call physicians are paid a per diem rate for each day spent on-call at the emergency department, except for one and one-half days that each physician must contribute gratis to the rotation schedule monthly (amounting to eighteen days contributed annually by each). It makes a difference if the on-call physicians must provide some days uncompensated or if they are paid for everyday of call. The former typically justifies a higher final rate.

“Unfortunately, many hospitals and health systems are only reactive to the question of call pay, rather than proactive.”
– Neal Barker
Questions that speak to patient volume, likelihood of being called, likelihood of having to present to the hospital, and patient complexity associated with each call, include:
- What is the average frequency of the physician presenting into the hospital (activations) per day when on-call?
- What is the average frequency of call interactions per day with hospital staff without presenting to the hospital when on-call?
- Is the facility trauma designated? If facility is trauma designated, what level of designation?
- Is the specialty’s call coverage required by trauma designation?
- Is the specialty’s call coverage required by any other designations/certifications (i.e., Certified Stroke Center, Heart Attack Center, etc.)?
- Is the call role first-call/primary physician or back-up physician?
- Are there “first-line” personnel (i.e., APPs, residents, fellows, tec.) available at the facility
to field/triage first calls and provide coverage support? - Please estimate the average time in the facility for the physician when called into the facility
- Degree of inpatient care typically required of the specialty for patients who initially present at the Hospital
- Required response time (time to facility)
- Number of hours per shift (Specify hours per shift (cannot exceed 24))
Financial burden is also key to the evaluation of call pay. OIG Advisory Opinions 07-103, 09-054, and 12-155 all address uncompensated care, and underinsured and uninsured patients that physicians encounter due to being on-call. OIG Advisory Opinion 07-10 is the OIG’s response to a medical center’s request for an advisory opinion regarding a physician on-call coverage and uncompensated care arrangement. In OIG Advisory Opinion 07-10, the OIG noted that “several features of the Arrangement appear to support the certification. The per diem rate paid to physicians appears tailored to reflect the burden on a physician and the likelihood that a physician in a particular specialty will be required to respond while on-call, as well as the likelihood that he or she will have to provide uncompensated treatment, and the likely extent of that treatment.” OIG Advisory Opinion 12-15 describes a favorable opinion of an arrangement in which, “physicians only will be able to seek payment for services rendered to uninsured patients.”
Clearly, financial burden is also recognized by the agency charged with evaluating and monitoring hospital-physician financial relationships to fight waste, fraud, and abuse with Medicare and Medicaid.
The following questions are intended to assist in evaluating a call rotation’s financial burden:
- Which party collects for professional services rendered when the Provider is called-in?
- Please provide the facility’s ED payer mix percentage for uninsured (self-pay) and Medicaid patients. The intent of this information is to determine the likelihood of having to respond to a request for ED or inpatient consultive services for an uninsured (self-pay) or Medicaid patient when on-call).
- Please provide the facility’s ED payer mix percentage for Medicare patients. The intent of this information is to determine the likelihood of having to respond to a request for ED or inpatient consultive services for a Medicare patient when on-call).
- Will the physician receive any additional production-based or fixed compensation per call-in?

“Hospitals and health systems’ need for call coverage isn’t going away, and isn’t getting any easier to secure or to manage.”
– Travis Ansel
Conclusion
Hospitals and health systems’ need for call coverage isn’t going away, and isn’t getting any easier to secure or to manage. Provided below are several key considerations for hospitals and health system executives dealing with the challenge that is call coverage.
- Set expectations with employed and independent physicians with medical staff bylaws that indicate a minimum number of days per month per physician that must be provided gratis, before call compensation can be considered. Only pay for extraordinary or disproportionate call days. For employed physicians, this could include tying an amount of base compensation to the provision of call coverage, and structure the employment agreement such that the amount can be withheld if the call coverage is no longer provided.
- Evaluate the burden of the call rotation and specialty in question based on questions such as the ones listed above to ensure that call pay is justified and needed, and that payment levels consider and reflect the burden of call.
- Consider a call pay structure that includes a low/conservative daily rate but provides an activation fee that is paid instances in which the physician must present to the hospital. This may be palatable to the physician, and less expensive over the long term for the hospital than a higher daily rate. In some situations, perhaps only an activation fee is needed. While many have found it difficult to manage, perhaps an “uncompensated care” arrangement is workable. Typically, in an uncompensated care arrangement, independent physicians that provide call coverage bill/invoice the hospital for uncompensated care provided to patients through the provision of call coverage.
- For employed physicians, especially those paid based on patient or Work Relative Value Unit (“wRVU”) production, do not forget that their receipt of compensation for each wRVU they produced is much different than an independent physician whose incremental payment for services rendered may be from an underinsured or uninsured patient. As such, when the physician or physicians providing call coverage are independent, payer mix is a significant consideration. The less favorable the payer mix, the higher the rate the on-call physician is likely to require.
- Additionally, for employed physicians, don’t forget that call pay is one component of total compensation that may include multiple components. If an organization has been aggressive with other compensation components (i.e., base, production, quality incentives, and medical direction), it may not have given itself much room for additional call pay. From a FMV and compliance perspective, be careful in aggressively stacking multiple compensation components on top of each other. In employed physician compensation design, the possibility of multiple components must be considered on the front end. Also, understand the market and survey data being utilized for benchmarking in compensation design and/or FMV assessment. Some surveys include call pay in reporting of total compensation, some do not.
