| This is the second article in a two-part series. The first covered best practices for adding advanced practitioners to physician networks. |
Three Tips on Measuring AP Productivity
Many employed provider networks have added advanced practitioners without tracking their direct and indirect contributions to productivity. This is a costly mistake and can be a hidden contributor to high practice losses. When measuring AP productivity, we suggest that you:
- Utilize survey data. Many organizations use survey data from MGMA, AMGA, or Sullivan Cotter to assist in physician wRVU measurement. These same surveys are increasingly including AP-related data. MGMA, for example, includes specialty-specific data for both nurse practitioners and physician assistants. This is important, because an orthopedic physician assistant’s wRVU-generating ability may be very different from a family practice nurse practitioner.
- Consider the practice model. While survey data is incredibly useful, APs vary in how they practice. Consider your practice model before establishing wRVU expectations. For an orthopedic PA, the MGMA median for wRVUs based on independent billings is 3,085. That may be unrealistic if your practice model doesn’t not allow independent AP billings.
- Focus on the team. There are practice models where the AP doesn’t generate independent billings, but contributes indirectly to overall productivity. An orthopedic PA, for example, may see post-surgery patients, allowing the physician to spend more time in the OR. In these cases, we recommend focusing on the provider team and establishing a team wRVU target to capture both direct and indirect contributions. For instance, if an orthopedic PA and physician are working together, a combined 11,326 wRVUs is reasonable, based on the median for each provider.
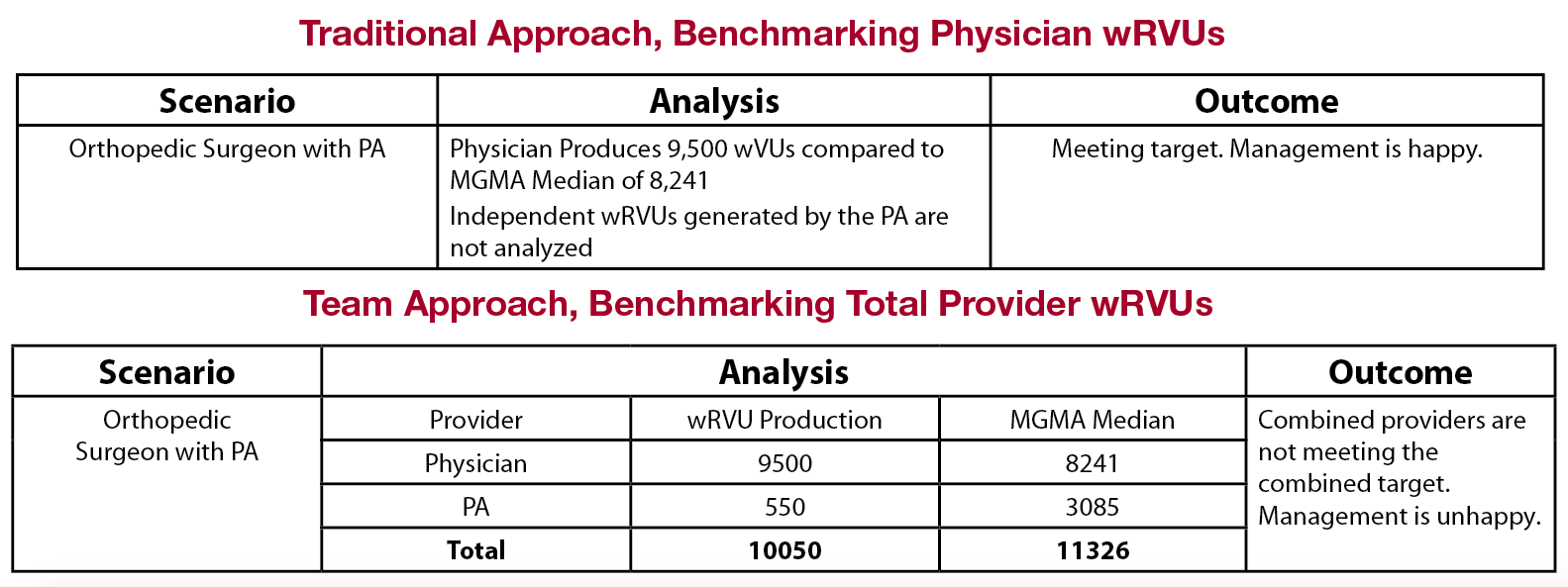
The above example shows how excluding the physician assistant’s indirect contributions from wRVU expectations can mask poor performance. Measured individually, the physician looks favorable to the median because of indirect productivity increases from the AP. However, the team approach reveals that the combined provider team is not meeting the combined target. This is a common situation for networks which seem to have high physician productivity, but still struggle with high practice losses.
Three Tips on Setting Compensation
APs play an important role in maintaining and increasing patient access to hospitals and healthcare systems. Establishing a compensation program that allows for successful AP recruitment and retention is critical to your success. Our most successful clients are following these tips:
- Utilize survey data (again). Just like wRVUS, specialty-specific compensation ranges are available for multiple provider types. Successfully hiring and keeping high quality APs requires market-based salaries consistent with the provider’s specific duties. Proper utilization of survey data will help ensure your total compensation package is both equitable and sustainable.
- Mirror your physician contracts. APs are providers and should be contracted and managed as such. We see many clients utilize base + wRVU + quality contracts for their physicians, while their APs are non-exempt, hourly-paid employees. These situations can create misaligned incentives and overall dissatisfaction. Instead, ensure all providers in the practice are striving toward the same productivity and quality goals. For practice models in which the AP bills independently, the AP should be eligible for wRVU-based productivity incentives. For team-based practice models, all providers should be held accountable to the combined wRVU target. In all scenarios, APs should be have quality incentives that mirror their physician counterparts.
- Stay legal. Physician compensation can be a minefield of regulatory and legal issues. Many of the key considerations, such as fair market value and commercial reasonableness, also apply to AP compensation. Ensure your organization has parameters in place governing the appropriateness of AP compensation.
