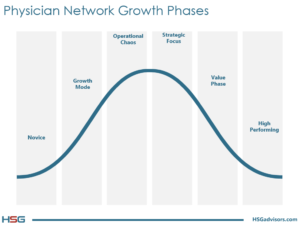
As depicted in the graph below, HSG believes that all hospital-owed physician networks progress along an evolutionary path, from “Novice” to “High-Performing”, with most struggling to emerge from Operational Chaos. HSG’s HFMA webinar on April 20, 2017, (click here to view) took a broad look at performance improvement and, specifically, a process to discover operational issues that have the network stymied and unable to move forward. This article focuses on an ancillary process that is often an outgrowth of a successful performance improvement initiative. That process is Physician Compensation Plan Redesign.
Often, the primary driver of network losses is a misaligned and poorly structured physician compensation plan. Because hospitals built their physician network infrastructure as they were progressing through the Novice and Growth phases, they’ve ended up with a disjointed compensation model that isn’t working anymore…perhaps never did. Too often organizations have multiple management personnel and executives structuring and finalizing physician contracts and compensation models without consistent structure or guidance. The result is Operational Chaos from a physician compensation perspective. The physician compensation structure of networks that are living this reality are typified by:
- High practice losses, hence an unsustainable compensation model;
- Compensation levels that far exceed production levels;
- No group or team culture;
- Complex models that are time-consuming and difficult to implement and manage;
- Low patient volume;
- Physician disengagement and apathy in operations and culture development; and
- Physician mistrust of management and the numbers that have a bearing their compensation.
What follows is a description of a process by which physician compensation can be successfully redesigned to yield the results you want and your network needs. The process will produce a compensation framework that accomplishes the following objectives:
- Receives buy-in and ownership from physicians;
- Supports the development of a cohesive culture within the group;
- Contains incentives related to production, as well as quality, patient satisfaction, citizenship, clinical process improvement, and/or teamwork;
- Maintains correlation between individual physician compensation and performance;
- Is competitive in the national marketplace while considering unique challenges within the market;
- Is financially sustainable going forward; and
- Provides a consistent framework and foundation with which the network can adjust to shifting revenue streams as value-based reimbursement models become more prevalent.
The Process
Develop a steering committee. The Physician Compensation Committee is charged with the task of leading the organization through a Physician Compensation Plan Redesign process. The committee should be comprised of 6 to 9 physicians, 2 to 3 advance practice professionals (if they will participate in the new plan), and 3 to 4 executives/administrators. The physician component of the committee should include representatives from the medical, surgical, and primary care specialty areas – perhaps 2 to 3 representatives from each.
Communication and education. Communicate the who, what, and why to all physicians within the group. To the steering committee, provide more in-depth education around national, regional, and local market factors influencing healthcare reimbursement, as well as other national, regional, and local factors that are affecting physician compensation. This educational session is likely to include details regarding Value-Based Purchasing in healthcare, MACRA, and MIPS, as well as background related to the Stark Law, Anti-Kickback Statute, and IRS 501(c)(3) regulations pertaining to hospital-physician relationships. It’s also extremely important to educate the committee regarding the organization’s current situation and the sense of urgency to streamline, standardize, and right-size physician compensation so the overall organization is better positioned to succeed in the future.
Complete a data review. Review and benchmark each physician’s current compensation levels versus his or her productivity levels (primarily Work Relative Value Units and collections) relative to industry benchmarks for their specialty. This will determine how each physician’s compensation relates and aligns to his/her productivity. We like to utilize a scatter diagram like the one presented below.
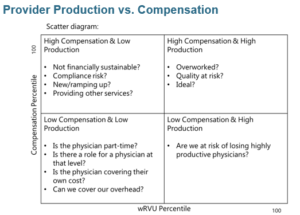
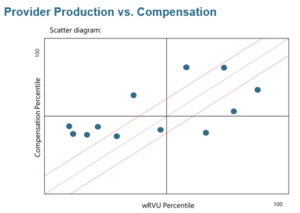
The scatter diagram plots compensation percentiles for individual providers on the y-axis and wRVU productivity percentiles on the x-axis. The resulting diagram gives a snapshot of the alignment, or rather misalignment, relative to productivity, of a network’s compensation structure. Obviously, this can be completed in various groupings as well (i.e., by practice, specialty, region, or service line). Note that we rarely find perfect alignment (i.e., 75th percentile production aligning with 75th percentile compensation) when practices are allowed to function organically, without outside influence, support, or subsidy (i.e., independent private practices). The economics do not change for hospital-owned practices either; in fact, they often get worse. Individual productivity tends to slow after acquisition/employment, practice overhead and operating expenses increase with the addition of robust hospital benefits for staff and physicians and investment in needed infrastructure (i.e., information technology). Therefore, it’s rarely feasible for production and compensation to have perfect alignment. We recommend a 5 to 10 percentile point lag, production over compensation—for example, wRVU production at the 75th, results in compensation at the 65th or 70th percentile.
Additionally, if available, we recommend a review of quality, clinical process, and patient experience data for the hospital and physician practices. This will establish baseline values for key quality, process, outcomes, and patient satisfaction metrics that can be integrated into the compensation plan. Since most organizations are not reimbursed for quality, process, outcomes, or patient satisfaction, such measures should not be the primary incentive of a physician compensation model. That said, because we know that reimbursement for these factors is likely to grow, it is probably a good idea to start small.
Contract Review. Review current employment agreements and compensation plans for each physician. Catalog key variables and terms for each contract into a detail compensation inventory or matrix. The matrix will allow you to identify commonalities, but most importantly, dissimilarities that need to be corrected. Not that every agreement is “cookie-cutter” or “boiler-plate,” but some limited variation and standardization in certain areas is a good thing and much easier to manage. Ultimately, there should be parameters around the most important terms and points of a physician contract.
Management and Physician Interviews. Conduct one-on-one discussions with key administrative and physician leaders, as well as selected advance practice professionals. Solicit their input to gain ownership of the new compensation plan, as well as invaluable insight as to what behaviors each stakeholder representative thinks should be incentivized. You will also learn what potential changes are likely to be major dissatisfiers before you head down a losing path.
One Size Does Not Fit All. Recognize the differences in practice type and specialty. Certain structures and incentives do not work in every situation. Most emergency medicine physicians and hospitalists are paid per an hourly or shift rate. This usually doesn’t make sense in a primary care practice. Likewise, productivity incentives may not make sense for a group of hospitalists when we want them to not exceed 17 patients per day because want to maintain high quality, outcomes, and satisfaction, and they have little control on the patient volume/referrals that are sent their way. Decide early in the process what needs to be incentivized and don’t force-feed incentives that are misaligned with the practice type.
Only Incentivize What You Can Measure. Too many times we’ve seen organizations incent quality, efficiency, patient satisfaction, and outcomes metrics that they can’t measure. The result is a pool of dollars that ends up being a giveaway that the doctors come to count on.
A successful physician compensation plan is never “cookie-cutter” or “one size fits all,” it considers incentives that are appropriate for the type of practice and it never gets too far ahead of the current reality by incenting performance that can’t be measured or is misaligned with current reimbursement schemes. In most cases, a well-structured, effective compensation plan ties compensation to performance in terms of both productivity, quality, and customer satisfaction, contains clear, measurable quality/outcome/satisfaction metrics that further the organization’s goals and objectives, are appropriately standardized across the employed network, and promote a shared group culture.
HSG is among the nation’s leading experts on physician compensation. If your compensation plan is at odds with network performance goals, call us. We can help.

